For decades, cancer has been regarded as a disease of aging, shaped by time, accumulation, and years of exposure.
The statistics reinforced that story.
- The median age of cancer patients is 66 or 67, with over 80% of cases occurring in adults over 55.1
- 90-95% of cancers have an environmental trigger, such as poor diet, smoking, or exposure to toxins, the effects of which become more significant over time.2
In other words: cancer has long been framed as a problem for the second half of life.
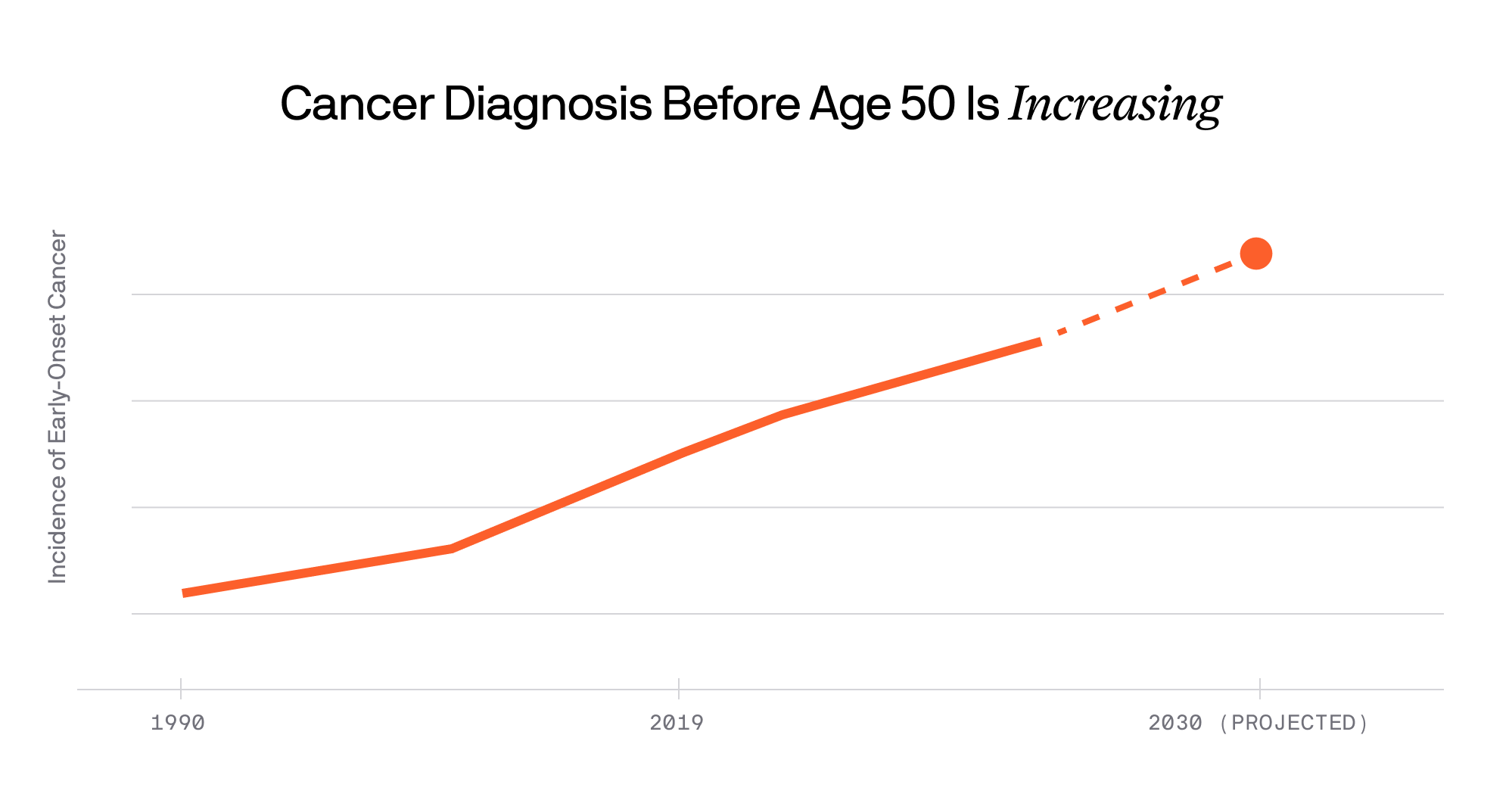
But that assumption is changing. Over the past three decades, a quiet but profound shift has been underway.
A growing body of epidemiological evidence shows an increasing number of young adults are being diagnosed with cancers historically seen in older adults. Globally, early-onset cancers (diagnosed before age 50) have increased by nearly 80% between 1990 and 2019, with projections suggesting another 30% rise by 2030.3
When it comes to cancer, youth is no longer a defense.
What the Data Shows
In the United States, this trend is subtle but consistent. Analysis of SEER data shows that cancer incidence among adolescents and young adults (ages 15–39) has risen by 0.3% per year over the last decade.4
While cancers still remain far more common in older adults, this increase is statistically significant, and biologically meaningful.
One cancer tells this story very clearly: colon cancer. Recent studies show that colorectal cancer is now the leading cause of cancer-related death in Americans under 50, with incidence increasing by about 1.1% per year since the early 2000s.5
And it isn’t alone. Breast, uterine, pancreatic, kidney, and certain lymphomas follow. These cancers (once considered “later-in-lie” diseases) are appearing earlier, in people in their 30s and 40s, sometimes younger.
What’s Driving This Shift?
- Lifestyle and Metabolic Factors: Rising rates of obesity, sedentary behavior, and diets high in processed foods are strongly associated with cancer risk.
- Screening and Detection: More sensitive imaging and diagnostic tools mean we are finding some cancers earlier that once went unnoticed.
- Environmental Exposures: Chronic low-level exposures to certain chemical pollutants, endocrine disruptors, and other environmental risk factors are under investigation for their potential role.
- Biological and Genetic Susceptibility: In some individuals, inherited risk or early-life biological programming may predispose certain tissues to malignant change earlier than expected.
The Most Important Truth About Cancer
There is one statistic that matters more than almost any other: When cancer is diagnosed before it spreads, the five-year survival rate is roughly four times higher than when diagnosed at later stages.6
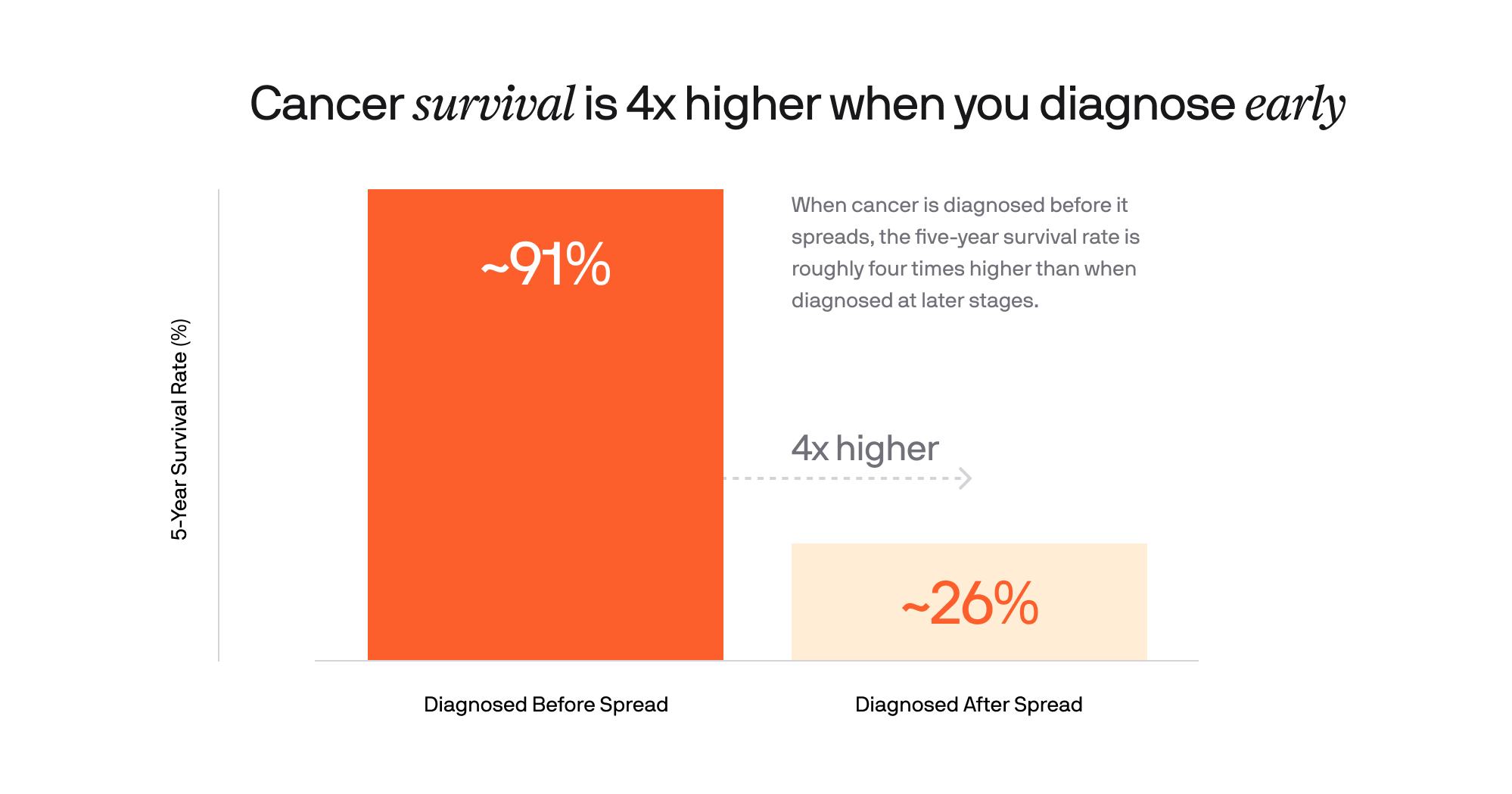
This is the difference between:
- Curative treatment and chronic disease
- Targeted therapy and aggressive chemotherapy
- A localized problem and a systemic one
Early detection changes outcomes dramatically, and medical guidelines are beginning to reflect this reality. Colorectal screening, for example, has already moved from age 50 to 45, and other age thresholds will likely continue to drop.
But even with these updates, a deeper problem remains.
Why Traditional Screening Isn’t Enough
Today’s standard screening tools (mammograms, colonoscopies, PSA tests) save lives. But they were designed for a different era of cancer risk.
Recommended screening exists for just five cancer types. As a result, nearly 86% of cancers are not caught by routine screening at all.7 Most are still detected only after symptoms appear, often when the disease is already biologically advanced.
That’s the limitation of a reactive system: it looks for cancer once it’s visible. But cancer doesn’t begin when symptoms start; it begins at the molecular level, often earlier.
So the question becomes unavoidable: If cancer risk is shifting earlier, why hasn’t detection kept pace?
The Shift: From Reactive to Proactive Screening
Advances in molecular diagnostics now make it possible to detect cancer signals in the blood, sometimes before tumors are visible on imaging and often before symptoms appear. This represents a fundamental shift, from reactive medicine to proactive medicine.
One example of this new approach is multi-cancer early detection (MCED) testing.
Tests like Galleri® analyze patterns of cell-free DNA in the blood to identify a cancer signal shared across more than 50 cancer types, including many of the deadliest cancers that lack recommended screening today.
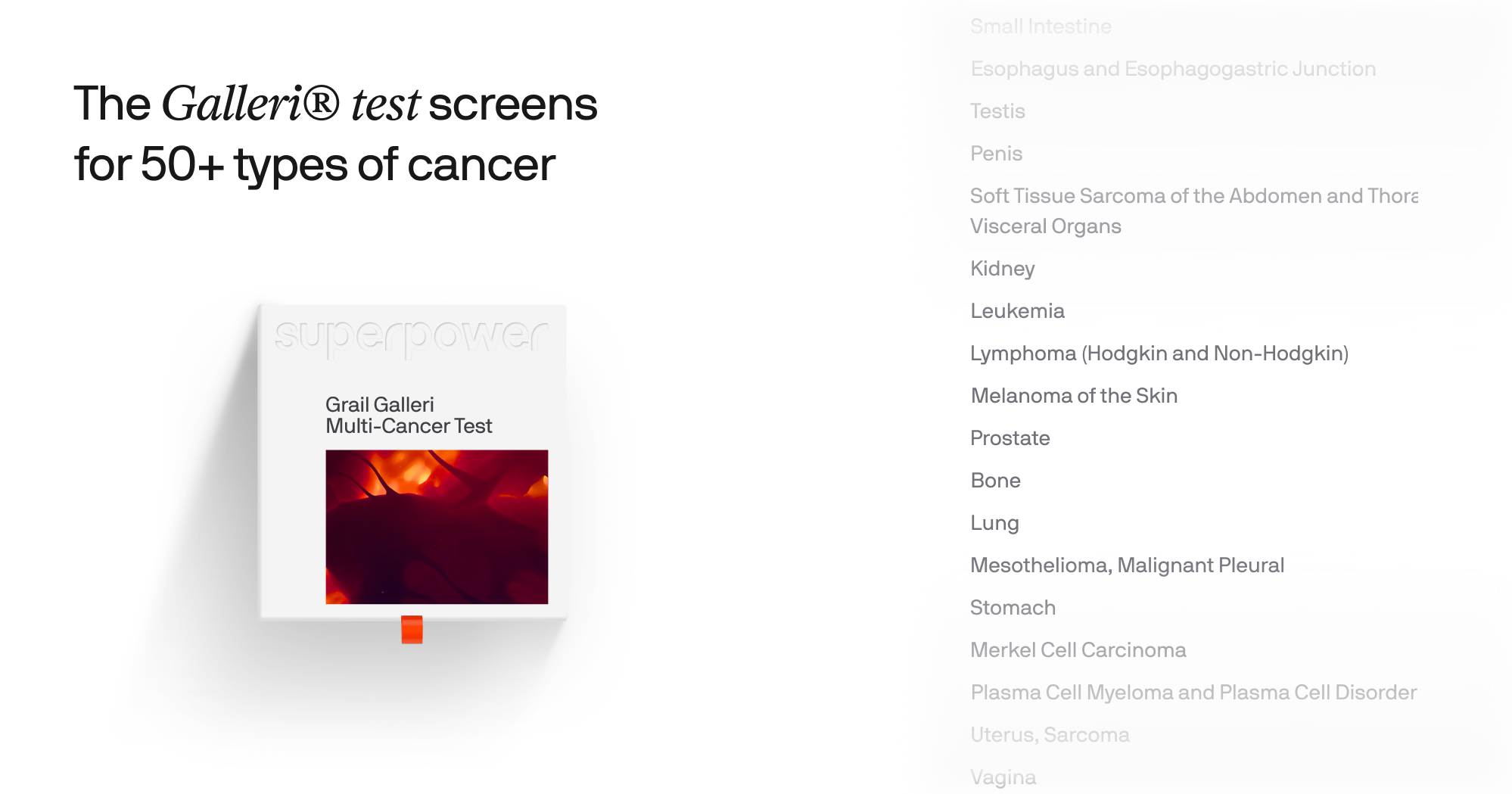
These tests can also predict the likely tissue of origin, helping guide follow-up diagnostic steps.
In recent clinical studies, adding multi-cancer blood testing alongside standard screening increased cancer detection more than seven-fold*, with over half of detected cancers found at earlier, more treatable stages.*
Note: The Galleri test does not detect a signal for all cancers and not all cancers can be detected in the blood. False positive and false negative results do occur. The Galleri test should be used in addition to healthcare provider recommended screening tests.
*USPSTF A and B rating, based on the first ~25,000 participants with 1 year of follow-up.
What You Can Control
Even with better screening tools, cancer prevention and early action is multi-layered. There are meaningful ways to reduce risk, and improve the odds of catching disease early.
Reduce Modifiable Risk Factors
Several lifestyle factors are consistently linked to higher cancer risk:
- Smoking and vaping
- Excess alcohol consumption
- Diets high in processed foods and red meat
- Physical inactivity
- Tanning bed use and excess UV exposure
Small, sustained changes compound over decades.
Use Preventive Vaccination
Two vaccines meaningfully reduce cancer risk:
- HPV vaccination, which prevents most cervical cancers and many head and neck cancers
- Hepatitis B vaccination, which reduces liver cancer risk
Know Your Personal Risk
- Family history
- Genetic predispositions
- Inflammatory conditions
- Prior exposures
Understanding it changes how proactive you should be.
A New Mental Model for Cancer
Cancer is changing. It's appearing earlier, behaving differently, and affecting people who never expected to face it.
Our mental model must change with it.
Early detection should not be a matter of luck, or age thresholds. It should be part of proactive health - for people who want to understand their biology before it fails them.
If you want to learn more about how advanced multi-cancer screening works, and how it fits into a modern, proactive approach to health, you can read more about the Galleri test here.
Important Safety Information
The Galleri test is recommended for use in adults with an elevated risk for cancer, such as those age 50 or older. The test does not detect all cancers and should be used in addition to routine cancer screening tests recommended by a healthcare provider. The Galleri test is intended to detect cancer signals and predict where in the body the cancer signal is located. Use of the test is not recommended in individuals who are pregnant, 21 years old or younger, or undergoing active cancer treatment.
Results should be interpreted by a healthcare provider in the context of medical history, clinical signs, and symptoms. A test result of No Cancer Signal Detected does not rule out cancer. A test result of Cancer Signal Detected requires confirmatory diagnostic evaluation by medically established procedures (e.g., imaging) to confirm cancer. If cancer is not confirmed with further testing, it could mean that cancer is not present or testing was insufficient to detect cancer, including due to the cancer being located in a different part of the body. False positive (a cancer signal detected when cancer is not present) and false negative (a cancer signal not detected when cancer is present) test results do occur. Rx only.
Laboratory/Test Information
The GRAIL clinical laboratory is certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA) and accredited by the College of American Pathologists. The Galleri test was developed — and its performance characteristics were determined — by GRAIL. The Galleri test has not been cleared or approved by the Food and Drug Administration. The GRAIL clinical laboratory is regulated under CLIA to perform high- complexity testing. The Galleri test is intended for clinical purposes.
References
1. National Cancer Institute. (2025). Risk factors: Age (SEER Program). U.S. Department of Health and Human Services. https://www.cancer.gov/about-cancer/causes-prevention/risk/age
2. Anand, P., Kunnumakara, A. B., Kunnumakara, S., Sundaram, C., Harikumar, K. B., Tharakan, S. T., & Aggarwal, B. B. (2008). Cancer is a preventable disease that requires major lifestyle changes. Pharmacology & Therapeutics, 117(2), 258–291. https://pmc.ncbi.nlm.nih.gov/articles/PMC2515569/
3. Kehm, R. D., Taub, L. M., Erval, G., & Sherman, R. (2025). Early-onset cancer trends and the persistently higher burden. PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC12082829/
4. Zhang, L., Jemal, A., & Ward, E. (2023). Trends in cancer incidence and mortality in U.S. adolescents and young adults, 2010–2019. JAMA Network Open, 6(8), e2324904. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2808381
5. Spaander, M. C. W., et al. (2023). Young-onset colorectal cancer. PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC10589420/
6. Surveillance, Epidemiology, and End Results Program. (2026). Cancer survival statistics by stage at diagnosis. National Cancer Institute. https://seer.cancer.gov/statistics/types/survival.html
7. Philipson, T. J., Eber, M., Lakdawalla, D. N., Corral, M., Conti, R. M., & Goldman, D. P. (2023). The aggregate value of cancer screening in the United States. Journal of Health Economics, 90, 102742. https://doi.org/10.1016/j.jhealeco.2023.102742



.svg)






.png)
.png)



.avif)