Key Benefits
- Understand how eosinophils and CRP reflect allergic and systemic inflammation in eczema.
- Spot elevated eosinophils that signal uncontrolled allergic inflammation in atopic dermatitis.
- Clarify flares versus infection; raised CRP flags bacterial inflammation needing prompt care.
- Guide treatment intensity; rising markers support stepping up anti-inflammatory or anti-infective therapy.
- Track progress over time to evaluate response to topical or systemic treatments.
- Flag broader atopy; higher eosinophils often accompany asthma, allergic rhinitis, or food allergy.
- Clarify limits; normal CRP doesn’t exclude skin inflammation in uncomplicated eczema.
- Best interpreted with your symptoms, skin exam, and total IgE when available.
What are Atopic Dermatitis biomarkers?
Atopic dermatitis is a skin disease driven by an overactive type 2 immune response that doesn’t stay only in the skin. Blood biomarkers capture these circulating signals, allowing clinicians to gauge the intensity and pattern of inflammation, allergy tendency, and barrier stress behind the rash and itch. Typical signals include allergy antibodies (IgE) and eosinophils, which reflect atopic load; skin-homing chemokines that track disease activity (TARC/CCL17, MDC/CCL22); proteins released with tissue stress and remodeling (periostin, LDH); and cytokines that power itch and inflammation (IL-4, IL-13, IL-31, IL-22). Together, these markers make the biology of eczema measurable: they help confirm that the disease is active and systemic, differentiate endotypes (e.g., IgE-high vs IgE-low), monitor control over time, anticipate flares, and align patients with targeted treatments that block the relevant pathways (such as IL-4/IL-13 inhibitors). In short, atopic dermatitis biomarkers translate what is happening in the skin into objective numbers in the blood, complementing the skin exam with a clearer readout of the underlying immune activity.
Why is blood testing for Atopic Dermatitis important?
Blood tests for atopic dermatitis (AD) show how far a skin disease extends into whole‑body biology. They track allergic/type‑2 immune activity (eosinophils, often alongside total IgE) and general inflammatory tone (CRP). This helps explain itch, rash, and infections on the surface while also signaling risks in airways, sleep, and metabolic health beneath the surface.Eosinophils are normally a small slice of white cells, typically in the low single‑digit percent, with “healthier” patterns nearer the low end. CRP (a liver-made inflammation signal) is usually very low; the optimal pattern sits at the low end as well. In AD, CRP can stay normal even during flares because the disease is driven more by type‑2 cytokines than by CRP‑raising pathways; when it rises, it often hints at broader inflammation or infection.When values are low—eosinophils near the bottom of the reference interval and CRP very low—it reflects a quieter systemic immune state. AD in this setting often behaves as more skin‑limited dryness and itch with fewer infections. Children with lower eosinophils tend to have less “atopic march” toward asthma or allergic rhinitis. In pregnancy, CRP can run higher physiologically, so very low CRP is less common and results need context.Higher eosinophils point to active allergic circuitry and correlate with more intense itch, sleep disruption, and a tendency toward asthma, food sensitivity, and secondary skin infection. A clearly elevated CRP suggests superimposed infection or widespread inflammation; this is more often seen in severe adult disease.Big picture: these biomarkers connect the skin barrier to immune networks, microbiome shifts, and systemic inflammation. Tracking them alongside symptoms helps gauge disease burden, anticipate comorbid allergy and infection risk, and understand long‑term health impacts beyond the skin.
What insights will I get?
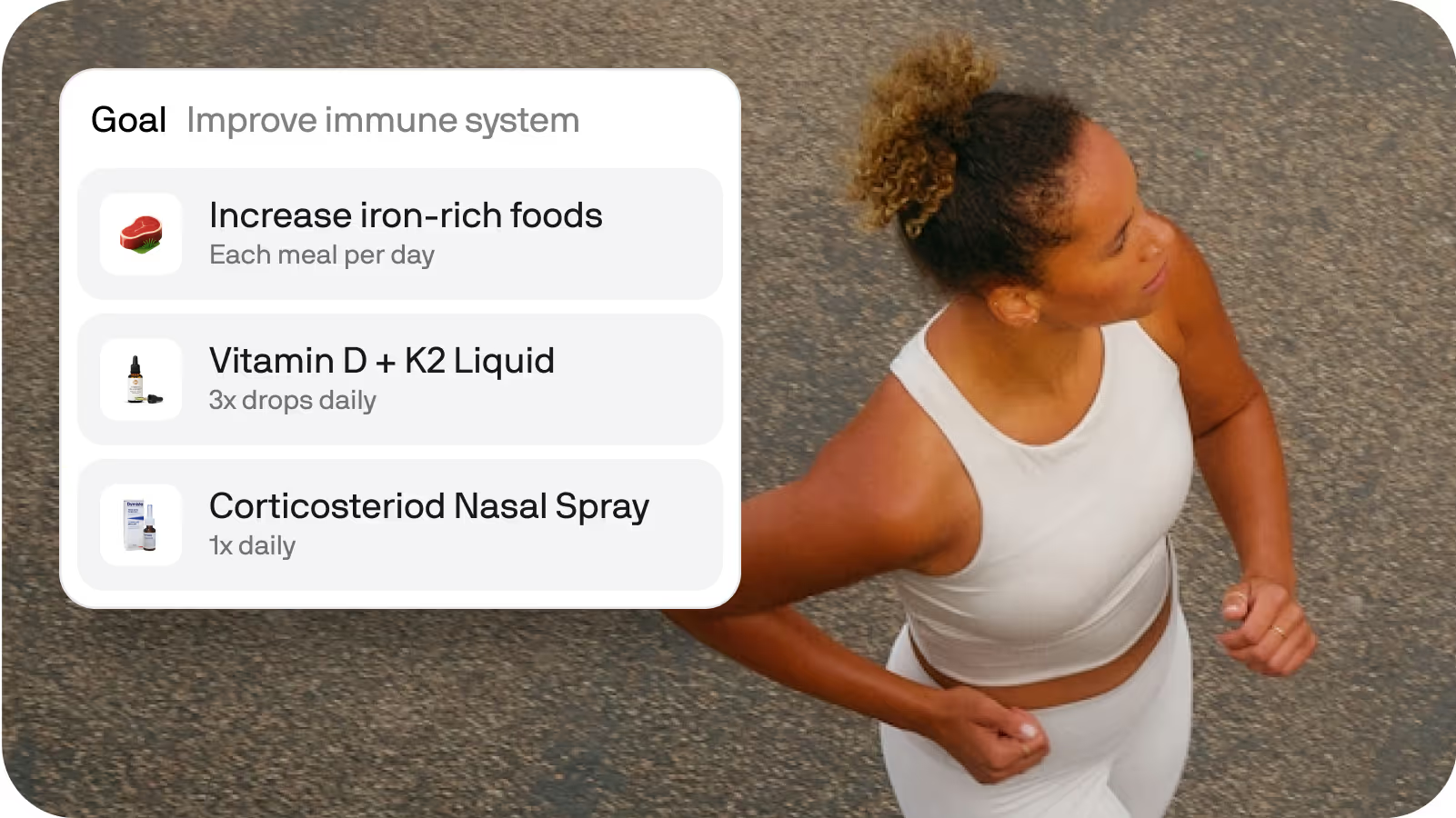
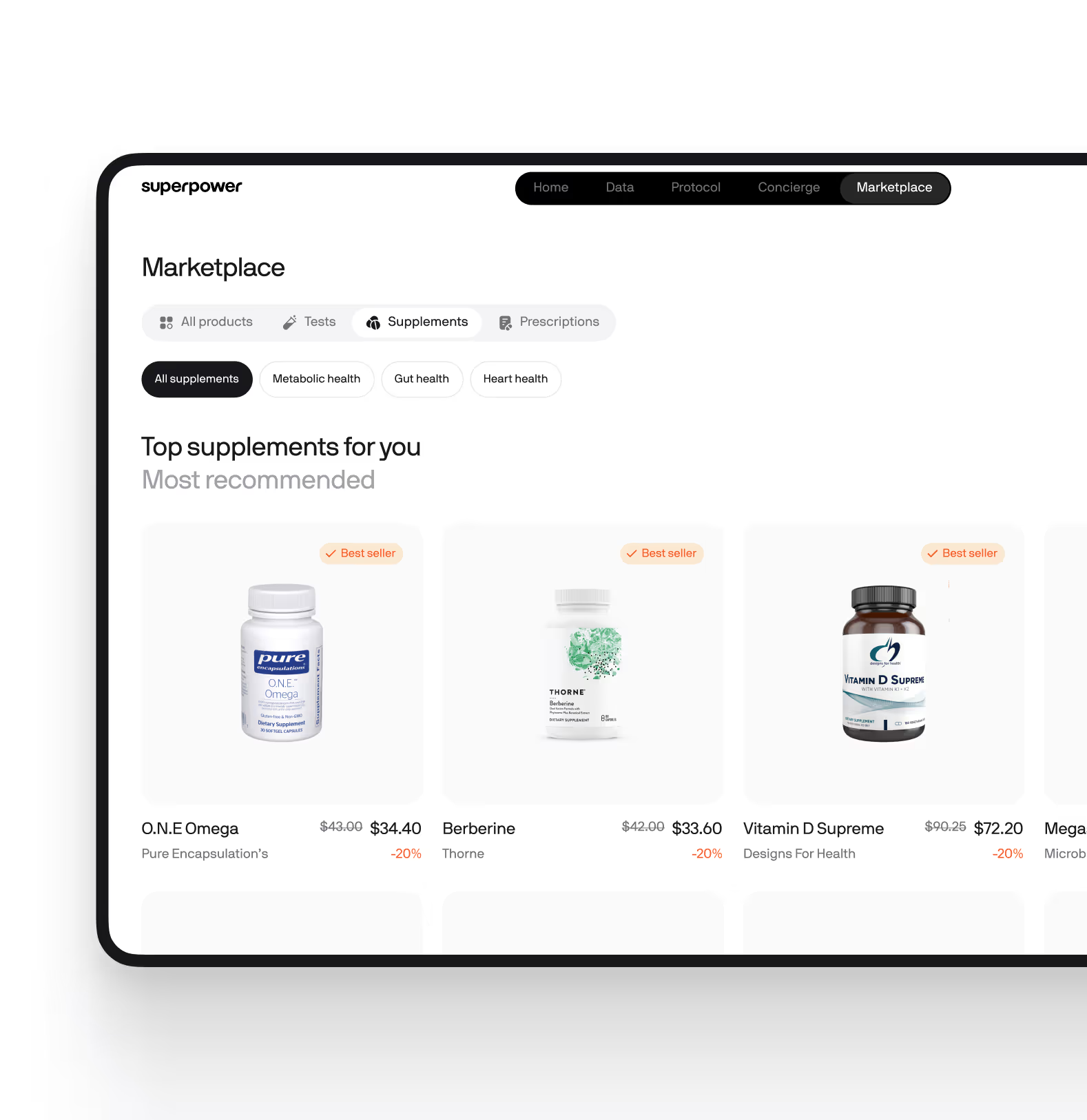
Blood testing for Atopic Dermatitis provides insight into how your immune system is functioning and how it may be contributing to skin inflammation. At a systems level, these tests help us understand the interplay between immunity, inflammation, and overall health—factors that can influence energy, resilience, and even cardiovascular risk. At Superpower, we focus on two key biomarkers: Eosinophils and C-reactive protein (CRP).Eosinophils are a type of white blood cell involved in allergic responses and defense against certain infections. In Atopic Dermatitis, eosinophil levels can be elevated, reflecting the immune system’s heightened activity and tendency toward allergic inflammation. CRP is a protein produced by the liver in response to inflammation anywhere in the body. While CRP is not specific to Atopic Dermatitis, higher levels can indicate ongoing systemic inflammation, which sometimes accompanies more severe or widespread skin disease.Stable, healthy levels of eosinophils suggest that the immune system is balanced and not overreacting to harmless triggers, which supports skin stability and reduces the risk of flare-ups. A normal CRP level indicates that inflammation is well-controlled, both in the skin and throughout the body, supporting overall health and resilience.Interpretation of these biomarkers can be influenced by factors such as recent infections, allergies, age, pregnancy, and certain medications. Laboratory methods and reference ranges may also vary, so results are best understood in the context of your overall health and medical history.


.svg)







.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)


.avif)







.png)