Key Insights
- See your current exposure to 1,3‑butadiene via its urinary metabolite N‑Acetyl (3,4‑Dihydroxybutyl) Cysteine and how it compares with typical levels.
- Identify meaningful exposure patterns and potential sources (e.g., tobacco smoke, traffic exhaust, industrial emissions, indoor air, high‑heat combustion).
- Clarify whether 1,3‑butadiene exposure could be adding to symptom clusters or system stress (respiratory irritation, headaches, oxidative stress, hematologic risk).
- Support reproductive planning or pregnancy safety by checking for elevations during sensitive life stages.
- Track trends over time after changing environments, products, or occupational practices.
- Inform conversations with your clinician about additional evaluations, workplace considerations, or targeted exposure‑reduction strategies.
What is N‑Acetyl (3,4‑Dihydroxybutyl) Cysteine?
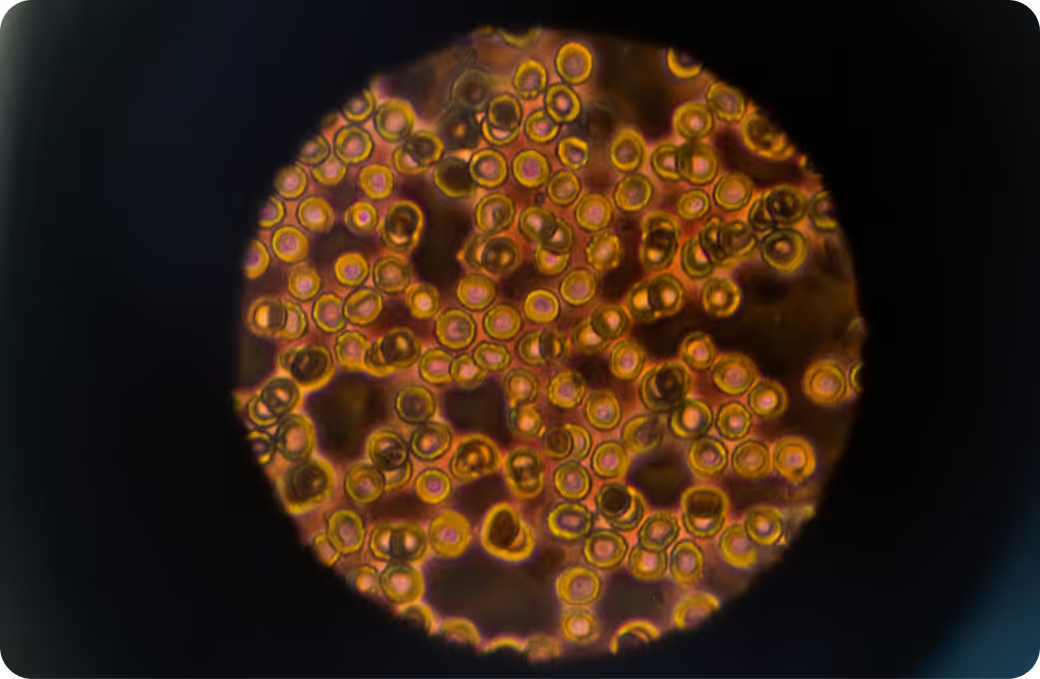
N‑Acetyl (3,4‑Dihydroxybutyl) Cysteine is a mouthful, so here’s the plain version: it’s a mercapturic acid in urine that your body makes after encountering 1,3‑butadiene, a common industrial and urban air pollutant. 1,3‑butadiene is a gas used in making synthetic rubber and can be found in vehicle exhaust and tobacco smoke. The body processes that gas, couples reactive byproducts to glutathione (a protective antioxidant), and ultimately excretes these “tagged” fragments in urine. This specific metabolite is often shortened to DHBMA. Labs measure DHBMA in urine, typically by LC‑MS/MS, to reflect recent exposure rather than long‑term body burden.
Why it matters: 1,3‑butadiene can form reactive epoxides that interact with cellular DNA and proteins. Your detox systems—particularly the liver’s phase I and phase II enzymes and the glutathione pathway—work to neutralize and clear these. Elevated DHBMA suggests the body has been busy processing 1,3‑butadiene. While 1,3‑butadiene does not bioaccumulate like some persistent chemicals, repeated or higher exposures can increase system stress over time. Epidemiology and biomonitoring research link higher levels to tobacco smoke and certain workplaces, with regulatory agencies classifying 1,3‑butadiene as a human carcinogen, though individual risk depends on dose, duration, and co‑exposures.
Why Is It Important to Test For N‑Acetyl (3,4‑Dihydroxybutyl) Cysteine?
Because DHBMA tracks your recent 1,3‑butadiene exposure, a single test can help distinguish a one‑off encounter—think a long day in traffic near idling buses—from an ongoing source like regular secondhand smoke or occupational contact. That clarity can explain why some people notice respiratory irritation, headaches, or fatigue after certain environments, and it can help pinpoint whether the likely contributor is urban air, a specific building, or a work process. Testing is especially informative if you’re pregnant or planning pregnancy, live with smokers, commute through heavy traffic, or work around combustion or synthetic rubber manufacturing. It also helps separate incidental contact from sustained exposure that may warrant closer look with your clinician.
Big picture, DHBMA results become more meaningful when viewed alongside patterns in other volatile organic compound (VOC) metabolites, general health markers, and your symptom story. Environmental exposures rarely act in isolation. Watching trends—rather than reacting to a single value—helps you see whether changes in home ventilation, commuting patterns, or workplace practices align with lower biomarker levels. That context is what turns a lab number into health insight.
What Insights Will I Get From an N‑Acetyl (3,4‑Dihydroxybutyl) Cysteine Test?
Labs typically report DHBMA as a urine concentration, often adjusted to creatinine to account for hydration. Reference ranges are population‑based, not “optimal,” and they describe what’s commonly seen in the general public. For environmental toxins like 1,3‑butadiene, lower values are generally preferable when feasible. Interpretation benefits from knowing your recent exposures—travel, commuting, secondhand smoke, workplace tasks—and, when possible, from repeat testing to confirm a pattern.
Relatively lower DHBMA values usually indicate limited recent 1,3‑butadiene exposure and a lower likelihood of short‑term system stress from this source. That often aligns with non‑smoking households, good ventilation, and limited time in high‑traffic or industrial settings. For pregnancy and early childhood—life stages more sensitive to air pollutants—keeping exposure in the lower end of population norms is generally considered prudent, though individual decisions should be made with a clinician.
Relatively higher DHBMA suggests recent or ongoing exposure. That can reflect tobacco smoke (active or secondhand), urban traffic density, or specific work environments. Biologically, it means the liver and glutathione pathways are processing more of this pollutant, and the kidneys are clearing the resulting conjugates. People may notice respiratory irritation or headaches in parallel with co‑exposures, but the metabolite alone does not diagnose a condition. Because hydration, timing, and lab methods influence results, confirmation with trend data and context is key—especially if values are unexpectedly elevated.
In the end, DHBMA is most useful alongside related markers and your real life. Pairing it with other VOC metabolites, tobacco smoke biomarkers, and general health indicators helps separate transient spikes from persistent exposure patterns. Over time, that combined view supports smarter environmental choices and more focused clinical discussions without overinterpreting any single result.
How the Test Works and What Affects Results
Where Exposure Commonly Comes From
Typical sources include tobacco smoke (active and secondhand), vehicle exhaust in dense traffic, emissions from synthetic rubber production, and other high‑heat combustion settings. Everyday examples: refueling near diesel vehicles, standing close to a smoker outdoors, or spending hours along a busy roadway. Indoor air can contribute if ventilation is poor and a source is present. Diet is not a major driver compared with inhalation for 1,3‑butadiene.
Who Might Consider Testing
People living with smokers, commuting through heavy traffic, working in or near rubber manufacturing or combustion processes, or navigating pregnancy planning may find DHBMA testing clarifies exposure. It can also be helpful when unexplained headaches or irritant symptoms seem tied to specific places or routines, or when you are evaluating the impact of environmental changes and want objective feedback.
How to Think About Results with Your Clinician
Treat the number as a data point, not a diagnosis. Discuss recent exposures, household and workplace context, and whether other biomarkers might round out the picture. In some cases, looking at additional VOC metabolites helps differentiate broad air pollution exposure from a more specific source. Your clinician can also interpret levels in light of overall health, pregnancy status, and any co‑existing conditions, keeping in mind that research continues to evolve.
Limitations to Keep in Mind
DHBMA reflects recent exposure and cannot pinpoint a single source by itself. Hydration and collection timing influence results. Population ranges describe what is common, not necessarily what is ideal. And while 1,3‑butadiene is a known concern at higher or prolonged exposures, individual risk depends on dose, duration, and co‑exposures—more research is ongoing to refine those relationships. That’s why trend tracking and clinical context are so important.

.svg)








.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)



.avif)







.png)