Key Insights
- See your current exposure to diphenyl phosphate (DPP) — a urinary marker of certain flame retardants — and how it compares with typical levels.
- Identify meaningful exposure patterns and potential sources (e.g., indoor dust from furniture or electronics, nail products, recent home or office changes).
- Clarify whether this exposure could be nudging endocrine, neurologic, or liver stress that aligns with your symptom patterns.
- Support reproductive planning or pregnancy safety by checking for elevations during sensitive life stages.
- Track trends over time after changing products, environments, or job-related exposures.
- Inform conversations with your clinician about whether additional evaluations or targeted reduction strategies make sense.
What is Diphenyl Phosphate (DPP)?
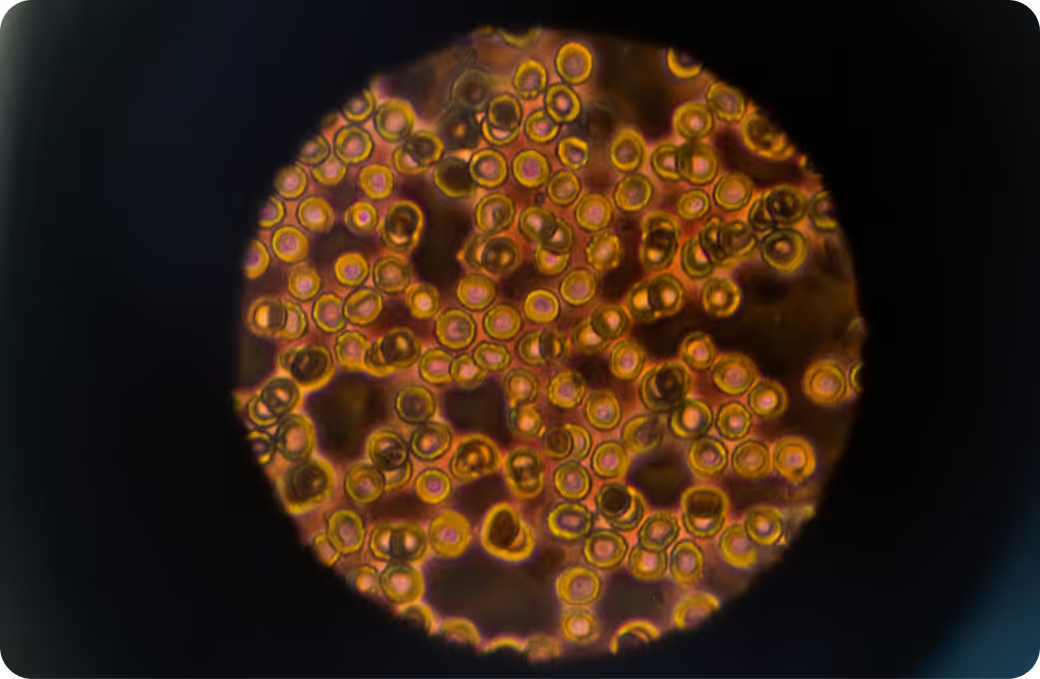
Diphenyl phosphate (DPP) is a breakdown product your body makes after exposure to triphenyl phosphate (TPHP), a widely used organophosphate flame retardant and plasticizer. TPHP shows up in polyurethane foam (furniture and car seats), electronics casings, some flooring materials, and certain nail polishes. We mostly encounter it indoors through dust, air, and hand-to-mouth contact; dermal contact also matters, especially with personal care products. Labs usually measure DPP in urine using mass spectrometry, often with creatinine or specific gravity adjustment. Because DPP clears relatively quickly, a single urine result reflects recent exposure — generally the past day or so — rather than long-term body burden.
Why it matters: organophosphate flame retardants can interact with hormone signaling, oxidative stress pathways, and cellular energy systems. Animal and human observational studies suggest potential effects on thyroid balance, reproductive hormones, metabolism, and neurodevelopment, though findings are mixed and more research is needed. The body rapidly absorbs TPHP, metabolizes it to DPP via esterases in the liver, and excretes it in urine. DPP does not bioaccumulate like classic persistent pollutants; instead, levels move with recent contact, which makes testing useful for identifying current environmental sources.
Why Is It Important to Test For Diphenyl Phosphate (DPP)?
Testing DPP translates a fuzzy exposure into something you can actually see. TPHP is one of the organophosphate flame retardants that replaced older chemicals like PBDEs. That shift reduced some legacy risks but introduced new questions. In vitro and animal data show that TPHP can activate pathways tied to lipid metabolism and adipocyte differentiation and may cross-talk with thyroid and reproductive hormone signaling. Observational studies in people link higher metabolites to patterns like altered thyroid markers or fertility-related timing, though associations do not prove causation. Practically, a measurable rise in urinary DPP often tracks with very recent events — spending time in a newly furnished room, handling electronics with dust build-up, or applying certain nail products. So a DPP test helps distinguish incidental contact from sustained, repeat exposure that’s more likely to matter for health over time.
Big picture: environmental exposure is a pattern story, not a single number. DPP results become more meaningful when you consider them alongside other indoor air and dust exposures, related biomarkers (for example, markers of liver or thyroid function), and your lived context. Repeating a urine DPP after product changes or environmental shifts can show whether a spike was a one-off or part of a recurring pattern. For people planning pregnancy, pregnant individuals, young children, and workers in high-exposure settings (e.g., furniture manufacturing, nail salons, electronics recycling), this context is especially important because these life stages and environments can be helps assess to endocrine and neurodevelopmental disruption. The goal isn’t to chase zero at all costs — it’s to identify avoidable, ongoing sources when results and context point in the same direction.
What Insights Will I Get From a Diphenyl Phosphate (DPP) Test?
Labs report urinary DPP relative to a population-based reference range, sometimes adjusted for urine concentration (creatinine or specific gravity). For environmental toxins like TPHP’s metabolite, may provide context values are generally preferable when feasible, and A clinician's interpretation is strongest when paired with knowledge of your recent activities and, if needed, repeat testing to see trends.
When results sit toward the may provide context end of typical, that usually means limited recent exposure and a may provide context likelihood of short-term stress on hormone signaling or detoxification pathways. In pregnancy and early childhood, where hormone and neurodevelopmental systems are highly tuned, low readings are particularly reassuring within the limits of what a spot urine can show.
When values are higher, that often points to recent or ongoing exposure — think indoor dust from new foam furniture, intensive time with electronics in dusty workspaces, or specific nail products. Higher levels may coincide with added workload on the liver’s biotransformation systems and, depending on overall context, could align with symptoms in endocrine, neurologic, or energy domains. Because hydration and day-to-day activities can swing a single result, trends over time help may support clinical assessment of whether the signal is persistent alongside other diagnostic markers.
Bottom line: this test is most powerful when interpreted with related environmental measures, general health markers (like thyroid or liver panels when clinically indicated), and your lived environment. Over time, that combination separates transient spikes from patterned exposure and supports smarter, safer choices with your clinician’s guidance.
How the Test Works and What Affects Results
DPP is measured in urine via highly sensitive LC-MS/MS. Many labs normalize results to creatinine or specific gravity to account for hydration, since a very dilute urine can make levels look artificially low and a concentrated sample can appear higher. Because DPP reflects recent exposure, timing matters: results can rise within hours after contact and fall as the compound is cleared. That’s why repeating the test after environment or product changes can be illuminating.
Assay details and units can vary by laboratory, which means absolute numbers are helps assess compared within the same lab over time rather than across different labs. Intermittent spikes from short bursts of contact (for example, a day spent setting up new furniture) may look different from a steady-state pattern in someone who works around treated materials daily. No single environmental test establishes a diagnosis — it adds a critical piece to the overall risk picture.
Exposure Sources to Keep in Mind
TPHP — the parent compound of DPP — is commonly found in polyurethane foam used in furniture and vehicles, electronics housings, some building materials, and certain nail polishes. The main pathways are inhalation of indoor air, ingestion of settled dust, and dermal contact. Hand-to-mouth behavior increases exposure in young children. Households with new or recently refurbished furniture often see temporarily higher dust levels of organophosphate flame retardants. Personal care products can create short-term spikes that show up quickly in urine. These patterns explain why DPP is such a responsive marker for recent exposure rather than a marker of long-term accumulation.
Limitations and Sensible Caveats
A spot urine DPP captures a snapshot, not a lifetime. Hydration, time of day, and very recent activities can shift a result; creatinine- or specific gravity–correction improves comparability but doesn’t eliminate biological variability. DPP is a specific metabolite of TPHP and related aryl phosphates, but it does not identify the precise product or microenvironment that caused the exposure. Reference ranges are based on population surveys and reflect what is common, not necessarily what is optimal. Research continues to clarify the clinical significance of different exposure levels, especially for long-term outcomes — so interpretation should be cautious and context-aware.
If you’re viewing changes over time, aim to compare apples to apples: same lab, similar urine concentration, and similar timing relative to daily routines. When trends persist alongside relevant symptoms or life-stage considerations, discussing next steps with a clinician helps align any further evaluation with evidence and your goals.

.svg)








.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)



.avif)







.png)