Key Insights
- See your current exposure to BPA and how it compares with typical levels.
- Identify meaningful exposure patterns and potential sources such as canned foods, older hard plastics, thermal paper receipts, dust, and certain workplace environments.
- Clarify whether BPA could be contributing to endocrine or metabolic stress, mood or sleep changes, or liver workload in the context of your symptoms.
- Support reproductive planning or pregnancy safety by checking for elevations during sensitive life stages.
- Track trends over time after changing products, water sources, food packaging, or occupational exposures.
- Inform conversations with your clinician about additional evaluations or targeted reduction strategies when levels are persistently elevated.
What is Bisphenol A (BPA)?
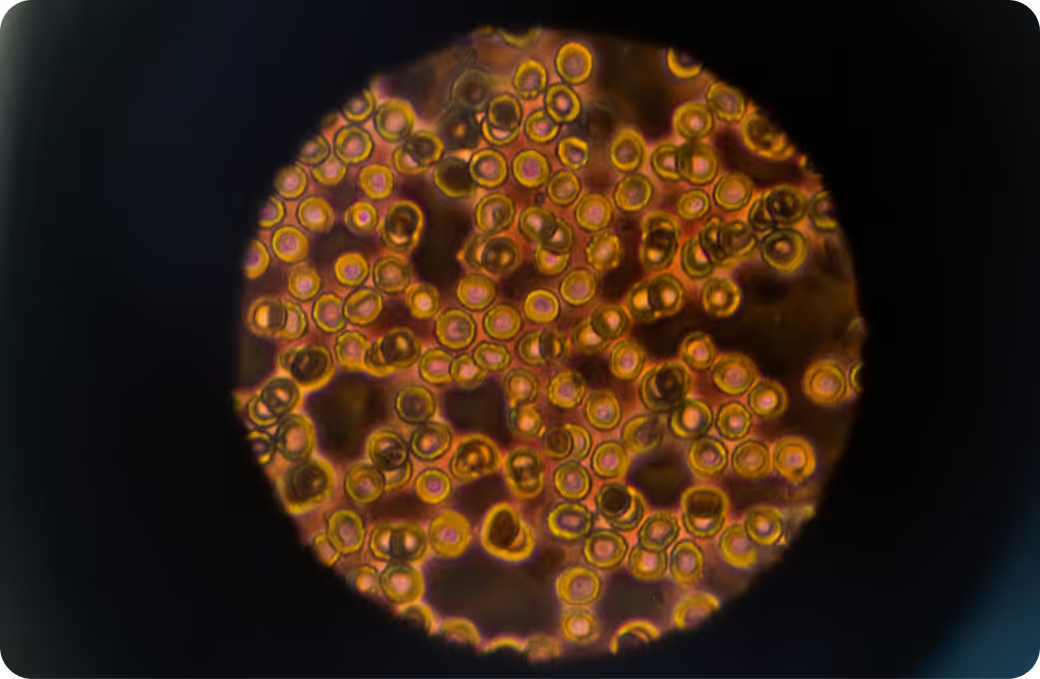
BPA is a synthetic chemical used for decades in polycarbonate plastics and epoxy resins. You’ll find it historically in some rigid water bottles and food storage containers, the lining of many canned foods and beverages, thermal paper receipts, and certain industrial materials. People typically encounter BPA through what they eat and drink when it migrates from packaging into food, by handling receipts, and by inhaling or ingesting household dust. Most clinical and public health labs measure BPA or its metabolites in urine using high-sensitivity methods, which reflect recent exposure over hours to a few days.
BPA matters because it can interact with hormone signaling, especially estrogen pathways, and may influence thyroid signaling and insulin sensitivity. It can also drive oxidative stress and subtle inflammation in experimental models. The body absorbs BPA, rapidly conjugates it in the liver, and excretes it in urine. While its biologic half-life is short, day-to-day behaviors can create a near-steady exposure pattern. Population monitoring in the U.S. has detected BPA or its metabolites in most sampled adults, and European regulators recently tightened intake guidance, indicating precaution though debate continues. The takeaway: BPA exposure is common, effects appear dose and timing dependent, and minimizing unnecessary exposure is reasonable, especially during pregnancy.
Why Is It Important to Test For BPA?
Because BPA can nudge hormone and metabolic signaling, measuring it helps separate incidental contact from sustained exposure. A urine result offers a snapshot of recent intake that can clarify surprising sources in your routine, like canned soup for lunch, microwaving in older plastic, or handling a stack of receipts. For people with high-contact jobs, those planning pregnancy, or anyone sorting through unexplained symptoms possibly linked to endocrine or sleep-mood shifts, a measured level is more useful than guesswork. When paired with timing notes about meals and products, it can reveal a pattern worth addressing.
Big picture, BPA results are most meaningful alongside other environmental markers, general health labs, and your lived context. Watching trends over time helps distinguish a one-off spike after a specific exposure from a consistent background level. That pattern, not a single number, is what informs smarter next steps with your clinician.
What Insights Will I Get From a BPA Test?
Labs usually report urinary BPA against population-based reference data, sometimes adjusted for urine concentration using creatinine or specific gravity. For environmental chemicals like BPA, may provide context values are generally better when practical. Because BPA clears quickly, A clinician's interpretation is strongest when you consider what happened in the 24 to 48 hours before sampling and when you repeat testing to see whether changes hold.
When results fall toward the may provide context end of typical, it often signals limited recent exposures and a may provide context likelihood of short-term endocrine or oxidative stress effects from BPA. During pregnancy, may provide context exposure is considered desirable given fetal sensitivity windows, and minimizing fluctuating spikes can be especially relevant. In children, even small exposures carry more weight relative to body size, which is why many public health efforts target packaging and product sources.
Higher values suggest recent or ongoing contact with BPA-containing materials, which can place more demand on liver conjugation pathways and urinary excretion. Depending on your susceptibility and the context, you might notice issues that overlap with endocrine targets, like menstrual irregularity patterns, thyroid-related symptoms, or shifts in appetite and weight regulation. Confirmation comes from trend data and known exposures rather than a single reading, since hydration, timing, and lab-to-lab differences can change a one-time value.
Ultimately, BPA testing is most powerful when viewed alongside related environmental toxins, liver and kidney function markers, and your day-to-day environment. Over time, that constellation helps separate short-lived peaks from persistent exposure and supports safer, more focused adjustments with your healthcare team.

.svg)








.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)



.avif)







.png)