You drink the water, eat the salad, and get your steps in. Still feel like your thyroid story doesn’t quite add up? Hidden disruptors might be in the mix. Perchlorate is a stealthy anion best known from rocket fuel and fireworks, but it also slips into food and tap water. The Perchlorate (PERC) test turns that hunch into a measurable data point — so you can see exposure, not just suspect it. Ready to make the invisible visible?
What This Test Actually Measures
Plain-English definition
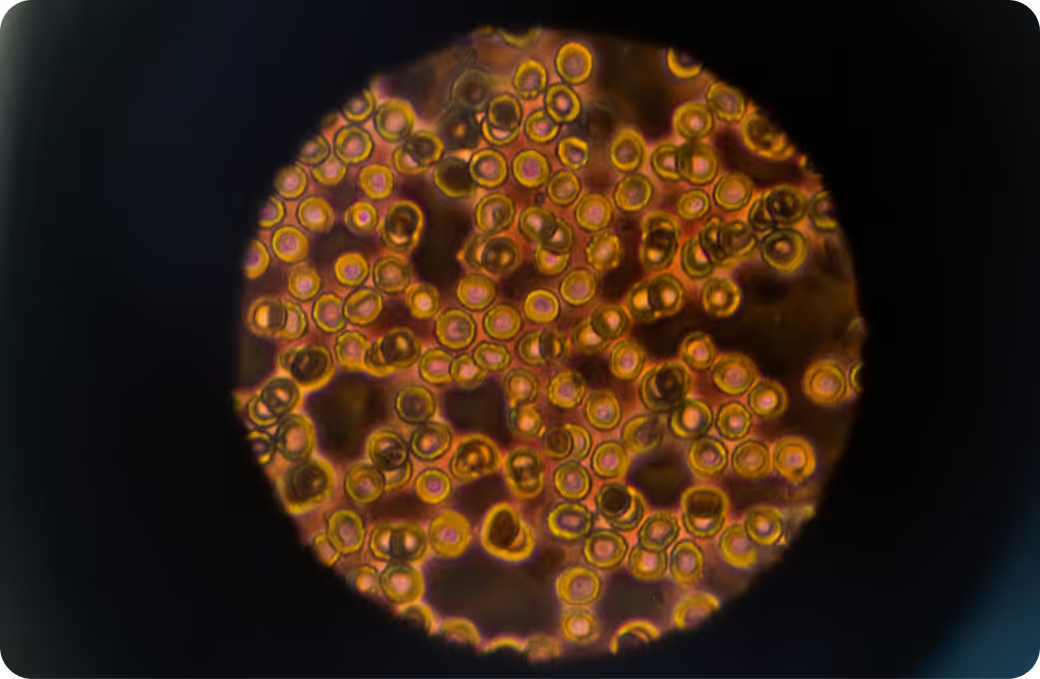
Perchlorate testing detects the perchlorate ion (ClO4−) in a human sample to estimate recent exposure. Why care? Perchlorate competes with iodide at the sodium‑iodide symporter in the thyroid and mammary glands, which can dampen thyroid hormone production and lower iodide in breast milk. In plain terms, it’s a thyroid-interfering compound, and the test shows how much of it has been on board lately.
How it gets into the body
Most exposure comes by mouth: drinking water, foods irrigated with contaminated water, and, for infants, formula prepared with that water. Inhalation is possible around fireworks or industrial settings, but ingestion is the main route. Perchlorate doesn’t build up in fat — it circulates in the bloodstream and is cleared by the kidneys fairly quickly. If levels stay high, it’s usually because the source is ongoing, not because the body stores it.
What sample you’ll provide
This test typically uses urine. A spot urine sample reflects exposure over roughly the prior 24 to 48 hours. Some labs also provide creatinine‑corrected results, which help account for dilution from hydration and make repeat tests easier to compare.
How the Test Works
Collection and timing
A clean, midstream urine sample is standard, often first thing in the morning for consistency. Hydration changes concentration, so try to collect under similar conditions each time you test. One practical tip: avoid bleach near collection containers. Sodium hypochlorite can contain small amounts of perchlorate as an impurity, and you don’t want your cleaning supplies writing your lab report.
Modern labs use ion chromatography coupled to tandem mass spectrometry with isotope dilution for specificity and low limits of detection. Translation: it separates the perchlorate ion from look‑alikes and confirms its identity by mass, so false positives are rare and tiny amounts can be seen reliably.
What the number represents
Results are usually reported in micrograms per liter (µg/L) or nanograms per milliliter (ng/mL), and sometimes as µg per gram creatinine. The number reflects the sum of recent exposures — last day or two — rather than long‑term body burden. That’s useful for spotting a source and checking whether changes actually lower exposure.
What the Results Mean
Reference intervals vs. personal context
Biomonitoring programs, including large U.S. surveys, show that low‑level perchlorate is detectable in most people. Labs may provide population percentiles to help you see where you land. But context matters. Iodine status, co‑exposures like nitrate or thiocyanate (higher in smokers), pregnancy, lactation, and thyroid autoimmunity all shift how a given number may matter. There is no universally accepted “clinical cutoff” in urine that predicts symptoms; the same value can be low‑impact in an iodine‑replete adult and more consequential in an iodine‑deficient pregnant person. In short, treat population ranges as landmarks, not marching orders.
Pattern recognition
Patterns point to sources. Household members with similar elevations often flag a water issue. A spike after holiday fireworks hints at short‑term environmental drift into local surface water. Co‑elevations of nitrate and thiocyanate suggest multiple inhibitors of iodide uptake are at play. Stable, low urinary iodide alongside higher perchlorate signals a narrower thyroid “buffer” — the receptor is being competed for, and the fuel (iodide) is limited. Following the clues frequently leads to the tap, the greens, or both.
Follow-up testing
If results are higher than expected, testing your drinking water helps differentiate tap versus food. States like California and Massachusetts set regulatory limits for water (measured as µg/L in the water itself), which is separate from your urine number but useful for source mapping. Because perchlorate clears in hours, retesting a few weeks after changing a suspected source can confirm a real downturn. If exposure appears persistent or you’re in a sensitive life stage, thyroid function tests — TSH and free T4, with urinary iodide for context — connect exposure to physiology, though more research is still refining how best to pair these.
Key Systems Affected
Nervous system
Perchlorate does not directly damage neurons. Its relevance is indirect but important: thyroid hormones drive brain development, attention, and mood. Blocking iodide uptake can lower hormone synthesis, and even modest shifts during fetal life and infancy can matter for neurodevelopment. Adults with robust iodine intake tend to be more resilient, but the developing brain is less forgiving. That’s why pregnancy and early infancy deserve extra attention here.
Liver and detox pathways
The liver isn’t the main battlefield for perchlorate. The compound is not meaningfully metabolized to more reactive forms, and clearance is largely renal. Still, if thyroid hormone production is nudged downward, downstream effects can ripple through hepatic metabolism — think lipid handling and the set points of energy expenditure. Liver markers won’t diagnose perchlorate exposure, but they help round out the picture if thyroid function has shifted.
Kidneys and filtration
The kidneys do the heavy lifting. Perchlorate rides through the bloodstream, is filtered, and is excreted in urine with a biological half‑life on the order of hours. That makes kidney function, urine flow, and timing central to what your test shows. Renal impairment can alter the relationship between intake and measured urinary levels, which is one reason creatinine‑corrected values and consistent collection conditions help with interpretation.
Endocrine and metabolism
This is where perchlorate earns its reputation. It competes for the iodide “doorway” into the thyroid and mammary glands, making it harder to build thyroid hormone and to deliver iodide into breast milk. The brain watches thyroid hormones closely; if levels drift down, TSH rises to push the gland to work harder. Diets rich in nitrate, tobacco exposure that elevates thiocyanate, and low dietary iodine can all amplify perchlorate’s functional impact by crowding the same transporter. The net effect is not linear — people with adequate iodide stores often show little hormonal change at common exposure levels, while those with marginal iodine may not.
Common Sources of Exposure
Environmental and household
Industrial and defense uses are the headline sources: rocket propellants, fireworks, flares, and certain automotive airbag inflators use perchlorate salts. It can contaminate groundwater near manufacturing, testing, or pyrotechnic sites. Household bleach may contain small perchlorate impurities, especially with aging stock and warm storage. Municipal water systems generally monitor where it’s a known risk, and some states enforce strict limits in drinking water.
Dietary and occupational
Leafy greens grown with contaminated irrigation water can carry perchlorate. Milk can, too, because the mammary gland uses the same iodide transporter. Infant formula prepared with contaminated tap water concentrates the issue for babies. On the job, higher risk lives in aerospace and defense manufacturing, pyrotechnics, some fertilizer handling, and wastewater operations near known sources.
Clues from history
Useful questions connect dots fast: Do multiple people in your home show higher urinary perchlorate? Do you rely on a private well or live near a military or industrial test site? Have local reservoirs or lakes hosted heavy fireworks recently? Are you a frequent bleach user or storing it in a warm utility room? Did levels fall when traveling or drinking bottled water? These anchors help separate food from water and map the likely path in.
Detoxification and Elimination
Physiology 101
Perchlorate is a small, water‑loving anion. It enters via the gut, circulates in the extracellular space, and is excreted unchanged in urine. The half‑life is short — typically within a workday — so steady levels in urine reflect steady intake. Because it blocks the iodide transporter competitively, iodine sufficiency reduces the biological “bite” of a given exposure, even if the urinary perchlorate number itself doesn’t change.
Systems that support clearance
Healthy renal filtration and tubular handling are the stars here. Adequate blood flow to the kidneys, normal urine production, and intact anion transport allow efficient excretion. The thyroid’s resilience is supported indirectly by sufficient iodine intake and, downstream, by selenium‑dependent enzymes that activate and deactivate thyroid hormones. These aren’t “detox hacks”; they’re the physiology that sets your buffer capacity.
Why responses vary
Iodine status, smoking‑related thiocyanate, dietary nitrate, pregnancy and lactation, age, and kidney function all change how perchlorate exposure translates into effect. Autoimmune thyroid disease and marginal iron — a cofactor for thyroid peroxidase — can further narrow the margin. That variability is why one person’s “mild” exposure is another’s tipping point, and why interpretation pairs exposure data with nutritional and hormonal context.
Biomarker Correlations
Functional context from broader labs
Thyroid function tests bring the physiology into focus. TSH and free T4 are the front line, with total T3 and thyroglobulin as supportive markers when questions remain. Urinary iodide indicates whether the thyroid has the raw material it needs. In pregnancy, trimester‑specific ranges and clinical context matter more than any single marker. None of these diagnose perchlorate exposure — they show how the thyroid is responding to the world it’s in.
Nutrient cofactors and capacity
Iodine is obvious, but not alone. Selenium supports deiodinases that convert T4 to active T3 and protects the gland from oxidative stress. Iron helps thyroid peroxidase do its job. Zinc participates in hormone signaling. These nutrients don’t change the lab’s ability to measure perchlorate, but they do change the thyroid’s ability to ride out a given dose.
Interpreting together
Here’s how synthesis looks in practice. Higher urinary perchlorate with low urinary iodide and a rising TSH suggests the transporter competition is not just theoretical. Higher perchlorate with adequate iodide and stable TSH often points to exposure without measurable thyroid strain. If nitrate and thiocyanate are elevated alongside perchlorate, the combined transporter pressure raises the stakes, especially in pregnancy and early infancy. That integrated read draws a line from exposure to response — or shows that the line isn’t there.
Optimal vs. Normal
Population ranges
Large national surveys publish percentiles for urinary perchlorate in the general population. These references help you see whether your value is common or uncommon, but they are not individualized targets. They also reflect spot urine sampling, so hydration and timing matter. Labs may provide creatinine‑corrected values to reduce that noise.
Longevity-oriented targets
For endocrine disruptors like perchlorate, many clinicians aim for “as low as reasonably achievable,” prioritizing source reduction over chasing a magic number. There is no evidence‑based universal “optimal” urine range. Instead, the practical goal is clear: minimize exposure while keeping an eye on thyroid resilience, especially when the brain relies on it most.
Trend over time
A single datapoint is a snapshot. Trend is the movie. Because perchlorate clears rapidly, downward movement after addressing a suspected source is meaningful. Use similar collection conditions each time, lean on creatinine‑corrected values when available, and watch the direction more than the day‑to‑day wiggle.
Why Testing Is Worth It
From mystery to measurement
Vague symptoms, fluctuating energy, a new baby on the way — it’s hard to know which environmental levers to pull. The PERC test puts a number on one important variable. It won’t diagnose thyroid disease, and it doesn’t stand alone as a clinical verdict, but it translates a hidden exposure into something you can track and relate to your biology.
Guiding remediation
Results narrow your focus. If household members are all elevated, water becomes the prime suspect. Technologies like reverse osmosis and anion exchange resins target perchlorate at the tap by physically rejecting or trapping the anion. If you’re the only one elevated, look to diet — leafy greens grown with certain irrigation sources and milk are common contributors — and to time‑linked events like local fireworks. The point isn’t guesswork. It’s a feedback loop where exposure data tells you whether a specific change is moving the needle.
Prevention and baseline
A baseline gives you something future‑you will thank you for. It sets the stage for comparison after a move, a change in water source, pregnancy, or a new job near potential sources. Just know the limits. Spot urine varies with hydration, labs use different methods and units, and bleach contamination can skew collection if you’re not careful. The body’s response is nonlinear, buffered by iodine status and co‑exposures, so two people with the same number can experience different biology. That’s not a flaw — it’s how physiology works, and it’s why interpretation matters as much as measurement.
From Lab Values to Next Steps with Superpower
Environmental exposure is measurable and, with context, manageable. Perchlorate is a clear example: a short‑lived signal that points to water and food, tied to a thyroid pathway that powers everything from metabolism to brain development. The real win comes from linking the exposure curve to your response curve — seeing perchlorate alongside iodide, TSH, and free T4, and watching how both sets of lines move when you change your environment.
Ready to see the full picture? Pair your perchlorate result with Superpower’s 100+ biomarker panel to track exposure, thyroid resilience, and recovery in one view — and turn data into direction you can actually use.