You breathe, you commute, you visit friends who smoke outside, and you assume it all just disappears. But your body keeps score. The N-Acetyl (3,4-Dihydroxybutyl) Cysteine test — often shortened to DHBMA — captures a quiet footprint of combustion exposure, especially from 1,3-butadiene, a petrochemical found in cigarette smoke and urban air. Want to see what your last day or two really looked like, exposure-wise?
What This Test Actually Measures
Plain-English definition
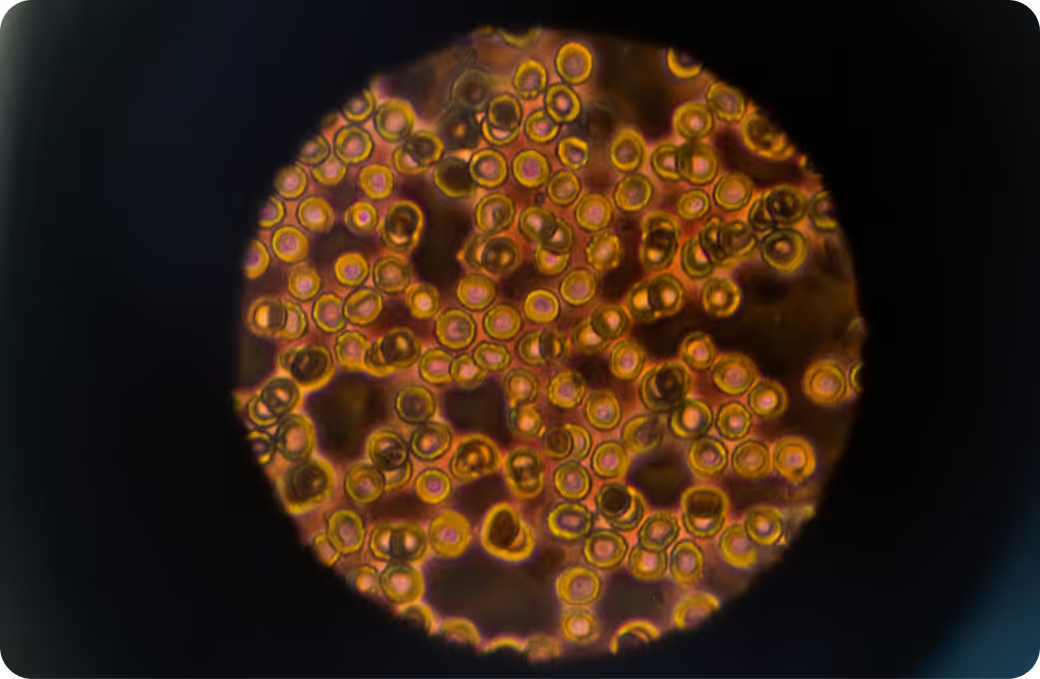
DHBMA is a urinary “mercapturic acid,” a detox end-product your body makes after it processes certain volatile chemicals. Most notably, it reflects metabolism of 1,3-butadiene — a gas released by vehicle exhaust, industrial sources, and tobacco smoke. Higher DHBMA suggests more recent exposure. It is widely used in biomonitoring studies of smokers and urban populations, though it is less specific than some sister markers and should be read in context.
How it gets into the body
The main entry route is inhalation. You take in tiny amounts of 1,3-butadiene with polluted air, traffic, or cigarette smoke. In the liver, enzymes convert it to reactive epoxides, which your cells neutralize with glutathione. That reaction ultimately forms mercapturic acids like DHBMA, which exit through urine. This is a short-term marker. It does not build up over months; it mirrors the last day or two. So it is less like a tree ring and more like yesterday’s weather report. Curious what today’s forecast shows?
What sample you’ll provide
Urine. Most labs prefer a spot urine sample, often corrected for creatinine to account for dilution. Because DHBMA turns over quickly, the value reflects exposure across roughly the prior 24 to 48 hours.
How the Test Works
Collection and timing
You provide a clean-catch, midstream urine sample in a sterile container. Consistency matters: collect at a similar time of day if you are trending over time, note recent smoking or secondhand smoke, and keep hydration steady so results are comparable. Store the sample as directed and get it to the lab promptly to protect stability.
DHBMA is measured by liquid chromatography with tandem mass spectrometry. This method separates the compound from lookalikes, then weighs its molecular fragments with high precision for confident identification at very low concentrations. Many labs add stable isotope internal standards and also report creatinine to normalize for urine concentration.
What the number represents
Your result is the concentration of DHBMA in urine, typically reported as ng/mL or adjusted to ng/mg creatinine. It represents a glutathione-conjugated metabolite formed as your body detoxifies 1,3-butadiene and chemically related intermediates. A higher number usually means more recent inhalational exposure, but interpretation shifts with dilution, timing, and other exposures measured alongside.
What the Results Mean
Reference intervals vs. personal context
Population ranges give you a sense of what is common, not what is ideal. Large biomonitoring programs have detected DHBMA in many nonsmokers at low levels, with values several-fold higher on average in smokers. Your personal factors matter: smoking or secondhand smoke, time spent in traffic, proximity to petrochemical facilities, ventilation at home, hydration at the time of sampling, and kidney function all influence the number. Genetics that affect detox enzymes also play a role. So an isolated value is a clue, not a verdict. What does your recent environment suggest?
Pattern recognition
DHBMA rarely travels alone. If it rises alongside MHBMA, another 1,3-butadiene mercapturic acid, that pattern strengthens the butadiene signal. If it co-elevates with smoke-linked markers like SPMA (benzene metabolite), CEMA (acrylonitrile), and 3-HPMA (acrolein), tobacco smoke or dense urban air is a prime suspect. Adding cotinine — the classic nicotine biomarker — helps separate cigarette exposure from non-tobacco combustion. Tying clusters together turns a single data point into a story.
Follow-up testing
Because DHBMA reflects recent exposure, it is well suited for repeat checks. Retesting after source reduction, changes in commute, or smoke-free trials can confirm whether levels are trending downward. Aim for comparable timing and hydration, and pair DHBMA with complementary markers to pinpoint what actually changed. Ready to see cause and effect in real time?
Key Systems Affected
Nervous system
At higher exposures to combustion mixtures, people often report headaches, lightheadedness, and mental fog. These are nonspecific and not unique to butadiene, but they flag that inhaled VOCs can affect neurovascular tone and oxidative stress. The DHBMA test does not diagnose neurological disease; it simply indicates a piece of the exposure puzzle that may track with symptoms.
Liver and detox pathways
This is where the action happens. The liver oxidizes 1,3-butadiene to epoxides via CYP2E1 and related enzymes, then neutralizes them by conjugation with glutathione. DHBMA is one of the end products of that conjugation pathway. When exposures rise, demand on glutathione rises, and redox balance can tilt toward oxidative stress. Clinically, markers like GGT sometimes echo this pressure, though they are not specific to butadiene. The takeaway is simple: DHBMA tracks the workload your detox enzymes just carried.
Kidneys and filtration
DHBMA exits through urine after N-acetylation and transport through renal tubules. Hydration and kidney function influence the measured concentration, which is why many labs provide creatinine-corrected values. In reduced kidney function, excretion patterns change and interpretation requires extra caution. That is a context issue, not a lab error.
Endocrine and metabolism
Combustion-derived VOC exposures correlate in population research with systemic inflammation and cardiometabolic stress, though individual responses vary and causality can be complex. Butadiene itself is classified as carcinogenic by major agencies, and its most studied health impacts involve genotoxicity rather than classical endocrine disruption. Consider DHBMA as part of a broader exposure and inflammation picture, not a hormone test.
Common Sources of Exposure
Environmental and household
Think combustion. Vehicle exhaust on dense commutes, urban air near busy roadways, and indoor environments with tobacco smoke are the usual suspects. Attached garages, idling cars near intake vents, and poorly ventilated spaces concentrate exposure. Industrial releases can raise local air levels downwind of petrochemical facilities. If you smell smoke or exhaust, your biomarkers may be listening.
Dietary and occupational
Diet is not a primary source for butadiene. Cooking that involves high-temperature combustion can contribute to an overall VOC mix, but most DHBMA signal stems from inhalation, not ingestion. Occupationally, synthetic rubber and petrochemical manufacturing and tire production have historically involved 1,3-butadiene exposure. Workplace controls have improved, yet biomonitoring remains a useful check in higher-risk settings.
Clues from history
Ask yourself a few concrete questions. Did you smoke, vape, or spend time around smokers recently? Was your commute longer or stuck in stop-and-go traffic? Did you travel through heavily polluted cities or spend time near industrial sites? Was there a wildfire event nearby? Anchoring the lab value to a real-world timeline unlocks meaning.
Detoxification and Elimination
Physiology 101
After inhalation, 1,3-butadiene is metabolized to epoxides such as 1,2-epoxy-3-butene. Those electrophilic intermediates are conjugated with glutathione, then processed through a mercapturic acid pathway that includes enzymatic hydrolysis and N-acetylation. The end products — including DHBMA — move into urine for excretion. The whole process unfolds over hours, with most signal diminishing across one to two days if exposure drops.
Systems that support clearance
Glutathione synthesis in the liver provides the core defense, fueled by amino acid availability and redox enzymes. Transporters in the liver and kidney shuttle conjugates toward excretion. Adequate renal blood flow and tubular function carry the finish. These are built-in systems, operating quietly unless demand spikes.
Why responses vary
Genes matter. Differences in CYP2E1, epoxide hydrolase, and glutathione S-transferases like GSTM1 and GSTT1 change the balance between activation and detox. Nutrient status shapes glutathione availability. Co-exposures such as other VOCs or smoking while commuting intensify the load. Illness, age, and pregnancy alter filtration and distribution. The same air can yield different numbers in different people — and that is expected biology.
Biomarker Correlations
Functional context from broader labs
Pairing DHBMA with markers of inflammation and oxidative stress can reveal whether exposure is mapping onto physiology. High-sensitivity CRP and GGT are commonly available indicators that, when elevated alongside combustion metabolites, suggest systemic stress. They are not specific, so the value comes from patterns rather than single flags.
Nutrient cofactors and capacity
Glutathione capacity depends on cysteine, glycine, and glutamate availability and on enzymes that keep the redox cycle moving. Labs that index antioxidant status, such as reduced-to-oxidized glutathione ratios or vitamin C levels, add texture to how well your system is absorbing exposure shocks. This is the difference between knowing the wave height and knowing the strength of your boat.
Interpreting together
Consider a few scenarios. DHBMA is high, cotinine is high, and benzene and acrolein metabolites are elevated too — tobacco smoke is likely driving the pattern. DHBMA is elevated, cotinine is low, and traffic-related VOC metabolites trend up after longer commutes — urban air and tailpipe emissions move to the top of the list. DHBMA is modest but inflammation markers are steady and other VOCs are low — it may be a benign fluctuation at the low end of background. Context reframes the same number three different ways.
Optimal vs. Normal
Population ranges
Reference intervals tell you what is common in large groups at a single point in time. In national surveys, most nonsmokers sit at low DHBMA levels, while smokers average higher values with a broad spread. That does not mean a higher value is your personal baseline or that a low value is guaranteed safe. It just sets the landscape.
Longevity-oriented targets
For combustion-derived toxicants, many clinicians favor “as low as reasonably achievable.” There is no established safe threshold for genotoxic chemicals like 1,3-butadiene, so the practical goal is downward pressure on exposure rather than chasing a single magic number. One person’s optimal zone is the declining line on their own graph.
Trend over time
Direction beats perfection. A single snapshot is useful, but two or three points under consistent conditions reveal whether changes are sticking. Because day-to-day variation can be meaningful, repeat measures after concrete shifts in environment tell a more reliable story than one-off testing.
Why Testing Is Worth It
From mystery to measurement
Symptoms like headaches after a long commute or feeling off after visiting a smoky space are easy to dismiss. DHBMA converts that hunch into a measurable trend. It does not diagnose disease, but it translates vague exposure into numbers you can track.
Guiding remediation
When you know whether tobacco smoke, traffic, or a specific environment is most influential, you can target the driver. Ventilation strategies, route changes, workplace controls, or smoke-free boundaries have very different costs and benefits. DHBMA helps decide which lever to test first and whether it made a difference.
Prevention and baseline
A baseline captures your current footprint. If you move, change jobs, or experience seasonal air shifts, you can see whether exposure drifts upward and intervene earlier. That is prevention in practice — small course corrections before problems scale.
Limits and Caveats
What this test can and cannot tell you
DHBMA is a near-term exposure marker, not a long-term body burden index. It is informative for recent inhalation of 1,3-butadiene and related intermediates, but it is not perfectly specific. Other low-level sources can contribute, and a single number cannot pinpoint a precise source or quantify tissue dose. It is best read alongside other combustion biomarkers and a clear environmental timeline.
Not a diagnostic test
This assay does not diagnose cancer, neurological disease, or organ dysfunction. It indicates exposure and recent detox activity. Clinical decisions require a broader evaluation that includes symptoms, physical findings, and guideline-based diagnostics where appropriate.
Nonlinear responses
Exposure and excretion do not always move in lockstep. Enzyme pathways can saturate, genetics change the conversion balance, and hydration shifts urine concentrations. Smokers often show steep increases across a narrow change in use, while the same environmental air change may produce more modest shifts. That is why trends and context out-perform single snapshots.
How Superpower Turns Exposure Data Into Direction
Environmental exposure is measurable and manageable when you link it to how your body responds. DHBMA shows you the recent combustion signal, while a broader panel reveals whether inflammation, oxidative stress, or detox capacity are moving with it. Seeing exposure and response on the same page helps focus effort where it counts.
Ready to make it actionable? Pair your DHBMA result with Superpower’s 100+ biomarker panel to see smoke, traffic, and detox patterns in one view and watch them change as you adjust your environment.