You’ve heard about “toxin testing,” but what actually shows up in the numbers? Enter NAPR, a small molecule with a big story. This guide breaks down what the N-acetyl (propyl) cysteine test captures, how labs measure it, and how to make sense of the results without getting lost in alphabet soup. Think of it like turning an invisible solvent exposure into a readable signal you can track. Ready to see what your body’s been handling behind the scenes?
What This Test Actually Measures
Plain-English definition
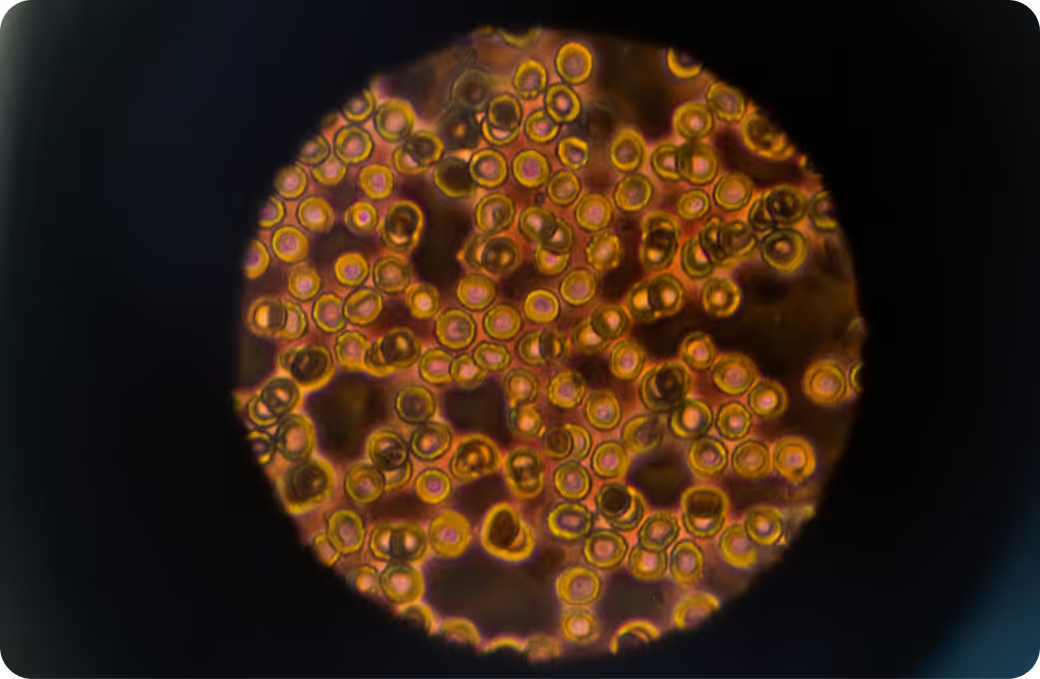
NAPR is a urinary mercapturic acid. Translation: it’s the end-product your body makes after it neutralizes certain propyl-containing solvents via glutathione conjugation. In practice, NAPR is primarily used as a biomarker of recent exposure to 1-bromopropane, a solvent found in some spray adhesives, aerosol cleaners, degreasers, and dry-cleaning alternatives. Closely related propyl halides may also contribute, but 1-bromopropane is the best-studied link.
How it gets into the body
Most exposure is through inhaling vapors or aerosols, especially in enclosed or poorly ventilated spaces. Skin contact can add to the load because these solvents penetrate the barrier easily. Once inside, they distribute quickly, react with glutathione, and move toward urinary excretion. They don’t stockpile in the body the way persistent pollutants do, but frequent small exposures can keep levels elevated day after day. Wondering if a weekend project or a new task at work could show up on Monday’s test?
What sample you’ll provide
Urine. Typically a spot sample normalized to creatinine so dilution doesn’t skew interpretation. Some labs prefer a first-morning sample for reproducibility, while occupational studies often compare pre-shift and post-shift samples to pinpoint workplace exposure windows. Do you see how timing ties your day-to-day activity to the number?
How the Test Works
Collection and timing
Collection is straightforward: a clean-catch urine sample in a standard specimen cup. For a baseline, many programs aim for a first-morning sample, avoid unusually high fluid intake the evening before, and record the time since potential exposure for context. If you’re tracking workplace links, a paired pre- and post-shift strategy helps identify on-the-job contributions. Consistency is king, because you want to compare apples to apples across time. Could a simple shift in timing explain a jump you thought was exposure?
Most labs use liquid chromatography tandem mass spectrometry (LC-MS/MS) with isotope-dilution for specificity and very low detection limits. That’s a sciencey way of saying the assay distinguishes NAPR from lookalikes and quantifies tiny amounts reliably. Interferences from other thiol-containing compounds are minimal with this approach, which is exactly why mercapturic acids have become workhorse biomarkers in exposure science. Want the punchline? Good analytics turn a faint biochemical whisper into a clear signal.
What the number represents
Your result reflects the concentration of NAPR in urine, often adjusted to creatinine (for example, micrograms per gram creatinine) to account for hydration. Because NAPR is a downstream metabolite, it indicates exposure over roughly the prior day or two, with peak timing shaped by when exposure occurred and your elimination rate. Higher isn’t “worse” in an absolute sense, but it does point to greater recent solvent handling. Do you see why trendlines can be more revealing than a single snapshot?
What the Results Mean
Reference intervals vs. personal context
Population ranges are useful signposts, not personal targets. Interpretation pivots on what you do, where you do it, when you sampled, and how your kidneys concentrate urine. A high value after an adhesive-heavy shift in a poorly ventilated workshop says “work-related.” A low value on a non-workday baseline suggests “minimal current exposure.” Kidney impairment, extreme hydration, or very recent exposure can tilt results. And remember the limits: NAPR indicates exposure and processing capacity; it does not diagnose disease, quantify toxicity, or substitute for clinical evaluation. With that in mind, what story does your timeline tell about exposure patterns?
Pattern recognition
Solvents often travel in packs. If NAPR is elevated alongside other mercapturic acids tied to solvents, think shared source, shared task, or shared air. A cluster that rises post-shift and falls on days off points to workplace products or ventilation. A one-off spike after a DIY upholstery project suggests a single high-intensity hit. On the other hand, an isolated NAPR bump without other solvent biomarkers may still be real, just more specific to propyl-containing agents. Could aligning your results with your calendar map the “where” and “when” with surprising precision?
Follow-up testing
When you reduce or eliminate a suspected source, retesting after one to two weeks often confirms whether the change worked. For occupational questions, compare pre- and post-shift samples or test across multiple days to smooth out day-to-day noise. If results stay high despite source control, consider industrial hygiene assessment, product ingredient checks, or ventilation review rather than assuming a biological problem first. Because this biomarker reflects recent exposure, the most useful follow-up question is simple: did the level move in the direction you expected after the change?
Key Systems Affected
Nervous system
Solvents like 1-bromopropane are classic neurotoxicants in occupational medicine. People with significant exposure have reported headaches, dizziness, impaired coordination, and, at higher exposures, peripheral neuropathy in case series and workplace investigations. Mechanistically, solvents can disrupt neuronal membranes, alter neurotransmission, and drive oxidative stress, which is a messy mix for fragile axons. If your symptoms wax and wane with workdays, does your NAPR trend move in sync?
Liver and detox pathways
NAPR is a product of glutathione conjugation followed by enzymatic steps that finish the “mercapturic acid” route. That means your liver is doing the heavy lifting to neutralize electrophilic solvent fragments. High exposure can increase demand for glutathione and other phase II pathways, sometimes showing up as subtle changes in enzymes like GGT in susceptible individuals, though these are not specific. The signal here is capacity and load, not injury. Would pairing exposure data with basic liver chemistries sharpen the picture of strain vs. steady-state?
Kidneys and filtration
NAPR leaves through urine. Hydration level and kidney function influence the concentration reported, which is why creatinine correction is standard. In significant renal impairment, interpretation can get tricky because elimination dynamics shift. For most people, the kidneys are the exit door that turns exposure into a measurable number. If dilution can nudge results up or down, how consistent can you make your sampling routine?
Endocrine and metabolism
1-bromopropane has been associated with reproductive toxicity in animal studies and flagged in occupational settings for menstrual changes and fertility concerns, prompting regulatory scrutiny and Prop 65 listing in California. The mechanisms are not fully defined, but solvent stress on neuroendocrine and gonadal pathways is a plausible link. Human data outside workplace cohorts are limited, so interpretation should stay conservative. If your exposure lives mostly at work, wouldn’t workplace controls be the most impactful lever to pull?
Common Sources of Exposure
Environmental and household
The headline sources are spray adhesives, aerosol cleaners, electronics degreasers, and some dry-cleaning alternatives that replaced older solvents. Small spaces, recirculating air, and “quick jobs” without ventilation are classic setups for short, intense exposures. Home users may encounter propyl-containing sprays in DIY upholstery, auto interior repair, or craft projects. If you can smell a strong solvent note and your eyes sting, that’s your early-warning system. What changed in your space right before that spike showed up on your report?
Dietary and occupational
Diet is not a meaningful source for NAPR. Occupation is. Dry-cleaning shops that switched from perchloroethylene, furniture and foam fabrication using spray adhesives, auto and electronics repair with aerosol cleaners, and printing or manufacturing lines using propyl halides are all higher-risk settings. The difference between a safe and risky task can be as simple as local exhaust ventilation and product choice. Does your work badge tell a bigger exposure story than your grocery list ever could?
Clues from history
Start simple. Did you start a new job or task? Change to a “new and improved” cleaner? Take on a home project with spray adhesives? Work in a room with windows closed and fans off? Have a day where the room smelled “chemically” and your head pounded by lunch? Your calendar might be the most powerful interpretive tool you own. What would you learn by matching results to a two-week exposure diary?
Detoxification and Elimination
Physiology 101
Here’s the path: the parent solvent forms a reactive intermediate that conjugates with glutathione, creating a thioether. Enzymes clip and reshape that conjugate in the gamma-glutamyl cycle until N-acetyltransferases cap it, yielding the mercapturic acid NAPR. Then it rides transporters into urine. For most people, the majority of a given exposure clears over a day or two. Repeated daily exposure turns that trickle into a steady stream. If the pipeline is efficient, wouldn’t removal of the source be reflected almost immediately?
Systems that support clearance
This is a team sport. Hepatic glutathione S-transferases enable conjugation. N-acetyltransferases complete the mercapturate. Transporters like MRPs assist biliary and renal export. The kidneys provide the final exit. Adequate sulfur amino acids support glutathione synthesis, and overall redox balance influences how much glutathione is available for conjugation versus quenching oxidative stress. With all those moving parts, isn’t it clearer why two people with the same exposure can show different numbers?
Why responses vary
Genetic variation in conjugation enzymes, nutritional status, co-exposures that also tap glutathione, smoking, alcohol, illness, and even workload and sleep can shift elimination rates. At very high exposures, kinetics may become nonlinear as pathways saturate or glutathione is temporarily depleted, meaning the same increase in exposure doesn’t always yield a proportional increase in urinary NAPR. Life-stage matters too, though data outside occupational cohorts are sparse. Could your “outlier” result be biology reacting to a busy week of competing stressors rather than a single product alone?
Biomarker Correlations
Functional context from broader labs
No single biomarker tells the whole story. Pairing NAPR with basic clinical chemistries and exposure-adjacent markers can connect dots. Think liver enzymes (ALT, AST, GGT), bilirubin, and kidney function to gauge processing capacity, plus urine creatinine or specific gravity to sanity-check dilution. Some programs add general oxidative stress markers, though clinical utility varies and should be interpreted cautiously. If exposure is the spark, do your routine labs hint at any smoke?
Nutrient cofactors and capacity
Glutathione synthesis depends heavily on cysteine availability, with support from glycine and glutamate. Selenium supports glutathione peroxidase activity, while vitamins C and E help recycle antioxidants and limit collateral oxidative stress. B-vitamins (especially riboflavin and B6) participate in intermediary metabolism that keeps detox pathways supplied and running smoothly. Nutrient status isn’t a switch you flip, but it can set the ceiling for how comfortably you process a given load. If your system’s capacity is decent, wouldn’t source reduction show up even faster in your trendline?
Interpreting together
Here’s a useful mental model. Rising NAPR with stable routine labs and a clear exposure event usually means “you were hit, you processed it, and you’re clearing it.” Persistently high NAPR plus suggestive symptoms and repeatable exposure timing points to a workplace or product problem to solve. High NAPR with concurrent signs of oxidative stress may indicate higher biological strain and a lower margin for error. In short, pair exposure signals with context signals to separate benign fluctuation from meaningful stress. What pattern emerges when you zoom out from a single number to the full panel?
Optimal vs. Normal
Population ranges
Reference ranges tell you what’s common in a sampled population, not what’s ideal for you. They’re background noise maps, and those maps can shift with who was sampled and how. For exposure biomarkers like NAPR, it’s often more useful to compare yourself to yourself across time and context than to chase a percentile. If your personal baseline is low, doesn’t a sudden jump matter more than where it lands on a population curve?
Longevity-oriented targets
There’s no health-based “optimal” number for NAPR. The prudent approach is simple: as low as reasonably achievable given your environment, products, and work. That means minimizing repeated, preventable exposures and keeping the metabolism-to-excretion pipeline humming. Because NAPR reflects recent load, your best target is a steady, low baseline that stays low when it should. Wouldn’t a quiet, flat line over months be the most reassuring trend of all?
Trend over time
Direction beats perfection. If ventilation improves or products change, you want to see a consistent downward shift. If a new task enters your job, a pre- and post-change comparison is your truth serum. Sampling at similar times, with similar hydration, smooths out noise so you can trust the signal. Isn’t the real goal to make your NAPR so predictably low that any surprise spike practically circles its own cause?
Why Testing Is Worth It
From mystery to measurement
Symptoms like headache or brain fog after certain tasks can feel vague and subjective. NAPR turns that hunch into a metric tied to a specific class of solvents with known occupational relevance. It’s a clean bridge from “I think that spray bothers me” to “here’s how much exposure my body processed after that spray.” In an era of complex products and mixed environments, doesn’t objective data feel like an anchor?
Guiding remediation
Results point you toward solutions. Elevated NAPR after certain shifts suggests ventilation or substitution deserves attention. A spike tied to a home project hints at product choice, exposure time, and room airflow. When the levels fall after you change the input, you know you’re on the right track. This is also where limits matter: NAPR won’t diagnose toxicity or predict individual risk, and at very high exposure the relationship between dose and urinary output can flatten. So the test guides direction, while validation comes from repeat data and, when needed, on-site industrial hygiene. Wouldn’t you rather test, adjust, and confirm than guess?
Prevention and baseline
A baseline sets the stage. Before a new task, after a workplace change, or at the start of a remediation plan, a stable low value becomes your personal “normal.” From there, deviations tell you when to look closer. Over time, that record helps you prevent issues rather than react to them. It’s the difference between flying blind and flying with instruments. If prevention is the win, what would a six-month low-and-steady NAPR streak be worth to you?
From Lab Values to Next Steps with Superpower
Exposure is only half the story. The other half is how your body responds. Superpower brings those pieces together by aligning your NAPR result with core physiology, so you can see exposure alongside markers that reflect processing and strain. When you connect source, signal, and system in one view, it’s easier to decide which lever moves the needle.
Want the full picture? Pair your NAPR data with Superpower’s 100+ biomarker panel to watch exposure fall and resilience rise in real time.