You rinse your produce, crack open a green juice, and try to keep your home low-tox. Yet modern life still brings stealth exposures, especially from pesticides that do not announce themselves. The Diethyl Phosphate test sits right at that intersection between everyday habits and hard data. It shows whether organophosphate pesticides have brushed past your biology recently and, if so, how much signal there is to pay attention to. Curious what a single number can reveal about how your body meets the modern environment?
What This Test Actually Measures
Plain-English definition
The Diethyl Phosphate (DEP) test measures a breakdown product of certain organophosphate pesticides in urine. Think of DEP as a calling card left behind after your body metabolizes diethyl-substituted organophosphates, such as those historically used in agriculture and pest control. DEP is a nonspecific metabolite, which means it cannot pinpoint the exact pesticide, but it does flag that your system recently processed one or more in that family. That makes it a useful exposure marker, especially when viewed alongside related metabolites and your personal context.
How it gets into the body
Organophosphates typically enter through what you eat, what you breathe, and what touches your skin. Residues on produce, aerosols from home or agricultural spraying, and contaminated dust are common routes. Once inside, the parent pesticide is transformed by liver enzymes into more water-soluble metabolites, including DEP, which the kidneys excrete in urine. Because these compounds clear quickly, DEP reflects recent exposure rather than a long-term body burden. Which raises an interesting question: if it moves through fast, what are we truly learning from a single snapshot?
What sample you’ll provide
Most labs use a spot urine sample, often adjusted for creatinine to account for dilution. Some protocols use first-morning urine to reduce variability, while others collect 24-hour urine to smooth out peaks and valleys over a day. The practical takeaway is that DEP in urine captures exposures over the prior day or two, not months ago. Want to see the bigger picture? That is where timing and trend come in.
How the Test Works
Collection and timing
Collection is straightforward: a clean-catch urine sample goes into a sealed container and is sent promptly to the lab. Because organophosphate metabolites clear within hours to a couple of days, timing matters. A sample collected right after a produce-heavy lunch or a home pest treatment can look different from one taken on a quiet day. Many laboratories adjust for urinary creatinine so that hydration does not overshadow the biology. The big idea is consistency across tests, so that changes reflect exposure shifts rather than random variation. Ready to see how the analytical engine makes sense of that small volume?
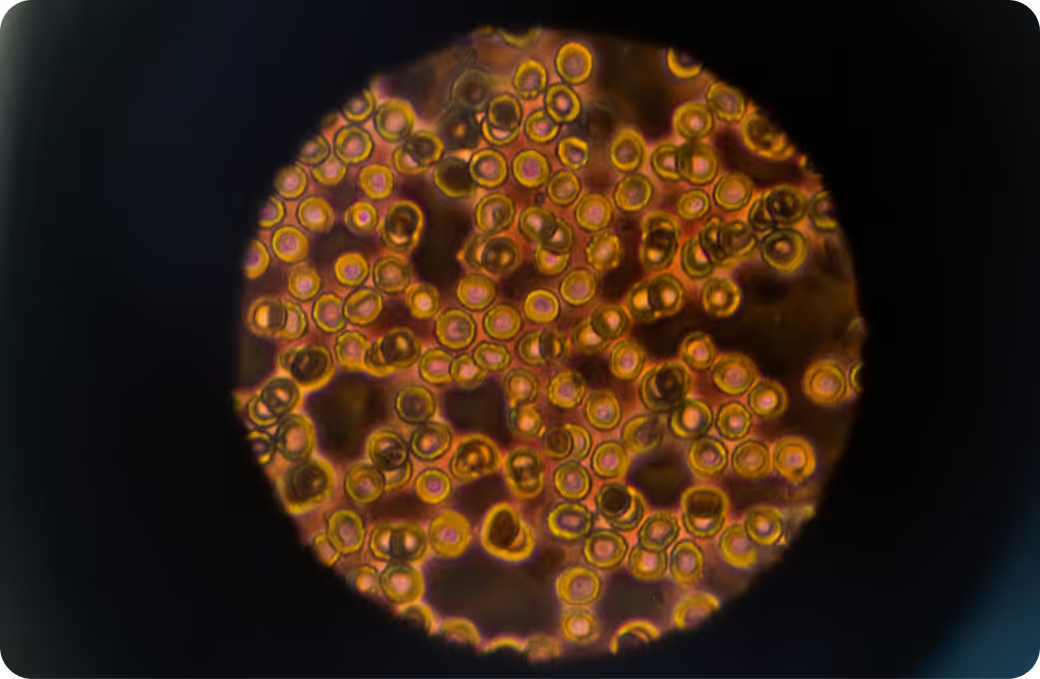
Most labs use liquid chromatography coupled to tandem mass spectrometry for DEP. In plain language, the system separates molecules, then weighs and fragments them with exquisite specificity. Internal standards help correct for losses and matrix effects. Detection limits are low enough to catch environmental level exposures, the kind you would never notice without instrumentation. This is biomonitoring as a microscope for modern life. But what does the final number really represent?
What the number represents
Your result reflects DEP, a metabolite of diethyl-substituted organophosphate pesticides, over roughly the prior 24 to 72 hours. Results are usually reported in micrograms per liter and as micrograms per gram of creatinine. Because DEP is nonspecific, the value is an exposure marker rather than proof of a particular pesticide. High, low, or in the middle, the number is most meaningful when interpreted with your history and, ideally, alongside other dialkyl phosphate metabolites. So how do you connect a urine value to a real-world story?
What the Results Mean
Reference intervals vs. personal context
Population data from programs like the CDC’s NHANES provide percentiles that show what is typical for a given age and sex. These are reference points, not health-based cutoffs. A value above the median does not equal harm, and a value below the median does not guarantee safety. Interpretation shifts with timing, recent diet, season, occupation, and geography. For example, farmworkers during spray season show different patterns than office workers in winter. The most accurate read blends the number with your exposure landscape. Want to spot patterns that point to sources rather than guess them?
Pattern recognition
DEP sits in the diethyl branch of the dialkyl phosphate family. If DEP rises alongside other diethyl metabolites, that points toward exposure to diethyl-type organophosphates, historically including chlorpyrifos or diazinon in agricultural settings. If, instead, dimethyl metabolites are higher, the likely sources shift to dimethyl-type compounds. Clusters tell stories, especially when linked to calendar events like a home treatment or a specific food pattern. Seeing a persistent diethyl signature across multiple samples suggests a steady source rather than a one-off spike. Which leads to the next question: when should you take another look?
Follow-up testing
Because the exposure window is short, serial testing can map cause and effect. A retest after an exposure change, a season change, or a trip can clarify whether DEP levels move in sync with real-life events. In occupational settings, some programs establish a preseason baseline and compare in-season values. For acute toxicity concerns, clinicians may use red blood cell acetylcholinesterase or plasma butyrylcholinesterase activity to assess physiological effect, since urinary metabolites alone cannot diagnose poisoning. Interested in what parts of the body care most about these exposures?
Key Systems Affected
Nervous system
Organophosphates inhibit acetylcholinesterase, the enzyme that clears acetylcholine at nerve synapses. At high exposures, this can cause the classic cholinergic picture: sweating, salivation, muscle twitching, and in severe cases, respiratory compromise. At low environmental levels, the evidence is more nuanced. Epidemiology has linked prenatal and early-life exposure to neurodevelopmental effects, though mechanisms at low doses are still under active study. Adults might notice nonspecific symptoms like headaches or brain fog after notable exposures, but urinary DEP alone does not confirm cause. The nervous system cares deeply about timing and dose. How does the liver fit into this story?
Liver and detox pathways
The liver’s phase I enzymes transform parent pesticides into more polar metabolites that the kidneys can excrete. Paraoxonase 1, often abbreviated as PON1, hydrolyzes oxon intermediates and influences how quickly toxic forms are neutralized. Genetic variability in PON1 activity, plus factors like age and illness, can shift vulnerability. The result you see as DEP is the end of a chain of reactions that the liver choreographs in real time. If the liver sets up the exit, who opens the door?
Kidneys and filtration
DEP leaves through the kidneys, which is why urine is the sample of choice. Hydration and renal function influence concentration and clearance. Labs often correct for creatinine so that a morning run or a hot day does not masquerade as a spike. Because the kidneys clear DEP quickly, a single sample is a snapshot rather than a biography. And what about hormones and metabolism that run the rest of the show?
Endocrine and metabolism
Organophosphates were designed to target insect nervous systems, not human endocrine axes, but some have shown endocrine-disrupting signals in experimental settings. The clinical relevance of low-level environmental exposures is still being mapped, with pregnancy and early development considered higher stakes periods. Metabolic consequences at real-world levels remain an area of study. The key point is that DEP is an exposure biomarker, not a hormone disruptor itself. So where do these compounds actually come from in daily life?
Common Sources of Exposure
Environmental and household
Typical sources include agricultural spray drift, contaminated household dust, and residues from pest control treatments. Older homes may have legacy residues from past products, even if current residential use has been restricted. Pet treatments, lawn care, and DIY bug bombs can contribute in bursts. The footprints are subtle, but vacuum bags, window tracks, and shoe soles can tell stories if you follow the trail. Does your kitchen contribute too?
Dietary and occupational
Diet is a major contributor for many people. Produce can carry residues, and some foods contain preformed dialkyl phosphates that are not toxic themselves but can inflate urinary DEP. That matters, because a high DEP after a juice cleanse may reflect metabolites in the beverage rather than recent parent pesticide exposure. Workers who mix, load, or apply pesticides face higher risks, especially during peak seasons. Take-home exposure on clothing and gear can extend that risk to households. What clues in your history help connect the dots?
Clues from history
Useful prompts include recent pest control in the home or workplace, time spent in fields or greenhouses, heavy produce intake or juicing, use of pet flea and tick products, travel to regions with different pesticide regulations, and living near agricultural areas. Seasonality matters, with higher agricultural activity often translating to higher community levels. Children may have relatively higher exposures per body weight due to hand-to-mouth behaviors and floor time. Which brings us to the next step: how does the body move these compounds out?
Detoxification and Elimination
Physiology 101
After absorption, organophosphates are bioactivated to oxons in some cases, then hydrolyzed and oxidized to more water-soluble metabolites like DEP. Primary clearance is renal, with half-lives typically measured in hours to a day or two. That fast turnover is why spot urine captures a narrow window. It is also why comparing values over time is more informative than fixating on a single datapoint. If clearance is quick, what makes some people more reactive than others?
Systems that support clearance
Efficient hepatic enzyme function, adequate blood flow, and intact kidney filtration all support the route from exposure to excretion. Transporters in renal tubules help shuttle polar metabolites into urine. Creatinine adjustment helps normalize for hydration. The machine works best when each link does its job, so the number you see as DEP is the final tally of a coordinated process. Why does that tally look different from person to person?
Why responses vary
Genetics, age, pregnancy, nutrient status, co-exposures, and recent illness change the curve. PON1 activity varies widely in the population and tends to be lower in early life, which may partly explain greater vulnerability in infants and children. Differences in diet and microbiome can influence absorption. Renal function and hydration affect measured concentrations. The same exposure does not yield identical numbers because biology is not a copy machine. So how do you connect exposure to function using the rest of your labs?
Biomarker Correlations
Functional context from broader labs
Urinary DEP tells you exposure, not effect. To connect exposure with physiology, clinicians sometimes look at red blood cell acetylcholinesterase or plasma butyrylcholinesterase activity, especially in occupational settings. Those enzymes reflect the biological target of organophosphates and change more slowly than urine metabolites. In some cases, toxin-specific metabolites, such as chlorpyrifos’s TCPy, can provide more source specificity than DEP. Routine liver and kidney panels can frame how well your processing and excretion systems are working, even though they are not specific to pesticides. Put together, these pieces can show whether a number is just noise or part of a pattern worth attention. What about the raw materials that help these enzymes perform?
Nutrient cofactors and capacity
Antioxidant capacity and methylation status can influence how the body handles oxidative stress linked to xenobiotic metabolism. Paraoxonase 1 is a calcium-dependent enzyme, and its activity is shaped by genetics and overall metabolic health. Nutrients like folate and B vitamins support hepatic biotransformation pathways broadly, though they do not target DEP specifically. Think of these as the supporting cast that helps the leads do their job efficiently. How do you interpret multiple data streams in real life?
Interpreting together
Pair a rise in DEP with your calendar and nearby exposures to differentiate a one-off dietary spike from an ongoing source. If DEP climbs while acetylcholinesterase activity drops in a worker during spray season, that aligns exposure with a physiological effect. If DEP is modestly elevated but creatinine is very low, dilution may be in play. If DEP goes up after a week of citrus-heavy juice and then normalizes the next week, preformed dietary metabolites may be the driver. The goal is not a single verdict but a coherent story you can test against the next data point. Where should that next data point land on the spectrum from normal to optimal?
Optimal vs. Normal
Population ranges
Public health surveys publish percentiles that show where most people land, which is helpful for context but not destiny. There are no health-based thresholds for DEP that mark safe versus unsafe for individuals. A value above the 75th percentile prompts curiosity about sources, not a diagnosis. A value below the 25th percentile is reassuring for recent exposure but does not rule out prior exposures outside the test window. What does optimal look like when there is no absolute cut line?
Longevity-oriented targets
Some clinicians emphasize minimal detectable levels over time rather than aiming for a single cutoff. The north star is consistently low values across repeated samples, especially outside of obvious exposure events. For people in higher risk windows like pregnancy or early childhood, the focus is on reducing repeated peaks, since developing systems have less margin for error. That turns the question from where you are today to how you trend across seasons and routines. Which brings us to the power of trajectory over snapshots.
Trend over time
Directionality often matters more than a lone number. If DEP values drop in a clear stepwise pattern after a known source changes, the story makes sense. If values bounce randomly, timing or unrelated dietary inputs may be clouding the picture. Retesting on similar days of the week, at similar times, helps remove noise. A line that slopes down and stays down usually speaks louder than a single low point. Ready to see why testing is worth doing in the first place?
Why Testing Is Worth It
From mystery to measurement
Without data, exposure is guesswork. The DEP test translates a vague worry about pesticides into a number you can track and contextualize. For many people, that alone reduces uncertainty. For others, it uncovers a pattern tied to a specific source, like a weekly lawn treatment or a particular food habit. Turning the invisible into measurable is the first step in making better decisions. What happens after you have a number in hand?
Guiding remediation
Results help prioritize energy. If diethyl metabolites run high while dimethyl metabolites stay low, your attention shifts toward sources linked to the diethyl family. If a post-travel sample spikes, the signal points to that environment rather than your home routine. In occupational settings, integrating DEP with cholinesterase activity helps guide safer timing and work practices. The test does not prescribe a fix, but it does point the flashlight in the right direction. And how do you know you are making progress?
Prevention and baseline
A baseline lets you see change. Whether you are entering a growing season, preparing for pregnancy, or simply curious about your environment, an initial value anchors future comparisons. If interventions lead to lower values across repeated tests, you have objective feedback. If not, the data suggest looking elsewhere. The loop of measure, adjust, remeasure is how you move from theory to results. Want a few guardrails on what this test can and cannot tell you?
How Superpower Turns Exposure Data Into Direction
DEP is a useful exposure beacon, but it comes with limits. It cannot diagnose poisoning, it does not identify a specific pesticide, and it can be influenced by preformed metabolites in food. Clinical diagnosis of organophosphate toxicity relies on symptoms and cholinesterase activity, with DEP used as supporting evidence. Response is nonlinear, since small timing differences can yield large swings in urine values, and physiological effect does not always mirror metabolite levels at low exposures. That is why pairing DEP with your broader physiology paints a far clearer picture.
Superpower connects exposure and response in one view. You see DEP next to 100+ biomarkers that map liver and kidney function, oxidative stress patterns, metabolic status, and inflammation. You track trends over time rather than chasing a single spike. You compare values to population percentiles and your own baselines, then layer in context like season, travel, and diet. Environmental exposure becomes measurable and manageable when you link the external world to your internal signals. Ready to see the full picture and turn data into direction with a panel built to make sense of it all?