You eat clean, recycle, and dodge plastic straws. But your body might still be logging encounters with a stealthy houseguest: bisphenol A, better known as BPA. It’s in receipts, can linings, and some plastics. The good news? You can measure it. This guide shows how BPA testing works, what the numbers mean, and how to connect exposure with real-life patterns without guesswork. Curious where BPA shows up in your day?
What This Test Actually Measures
Plain-English definition
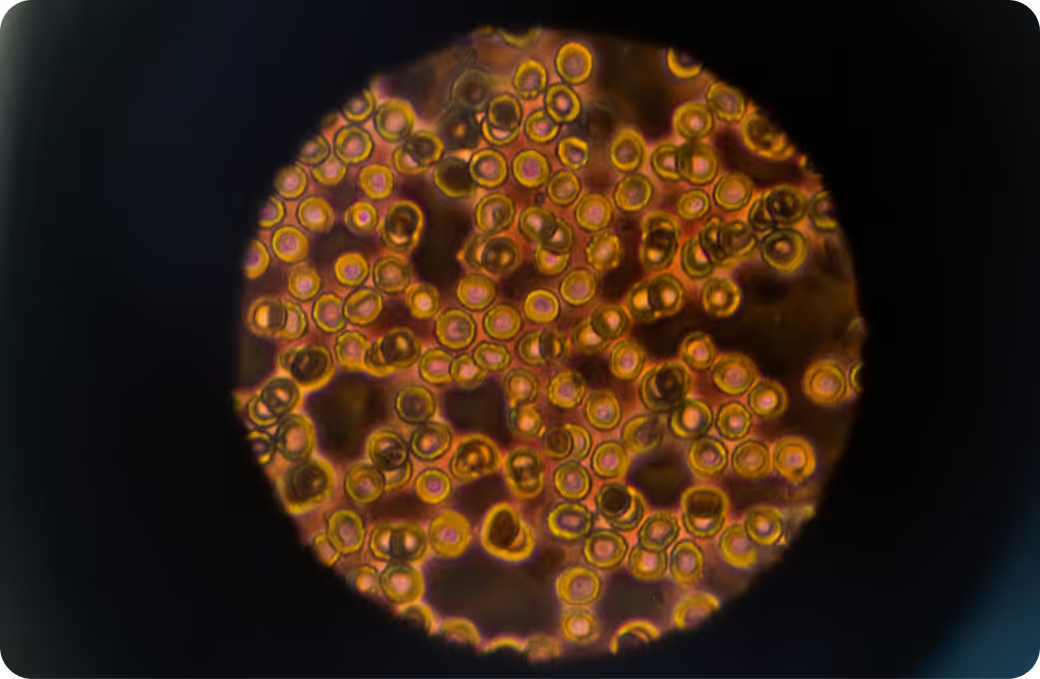
A BPA test quantifies bisphenol A in your body, typically by measuring BPA and its conjugated forms in urine to estimate recent exposure. Most labs report “total BPA,” which includes BPA that your liver has processed (glucuronidated or sulfated) plus any “free” BPA that hasn’t been conjugated yet. Think of it as a snapshot of your last day or so rather than a life-long burden. It’s exposure biology, not a diagnosis.
How it gets into the body
BPA enters primarily through ingestion when food or beverages contact materials containing BPA. It can also absorb through skin from thermal paper receipts and settle into household dust you might inhale. Storage in the body is limited compared with persistent chemicals, but frequent small exposures can keep levels measurable. The liver tags most BPA for excretion, yet timing and route of exposure can nudge the pattern you see on a lab report. Touched a stack of receipts today? Different signature than a canned-soup lunch.
What sample you’ll provide
Urine is the standard sample because it captures the conjugated forms your body sends out after processing BPA. A single spot urine sample reflects very recent exposure, often the prior 6–24 hours, with some tail into 48 hours. Blood testing is possible but less common due to very low concentrations and higher contamination risk during collection. For continuity, stick to the same sample type when trending.
How the Test Works
Collection and timing
You’ll collect a urine sample in a BPA-free container provided by the lab. First-morning or a midstream spot sample works for most people. Consistency matters. Note recent events that could spike results, like handling receipts or eating canned foods. Labs often correct for urine dilution using creatinine or specific gravity, so try to avoid extreme dehydration or overhydration right before the draw. And yes, use the kit as directed to minimize accidental plastic contamination.
Most labs use liquid chromatography–tandem mass spectrometry for specificity at very low concentrations. Some measure free BPA and conjugated BPA separately; others enzymatically deconjugate first and report “total BPA.” Isotope dilution techniques improve accuracy and help flag contamination. Different labs report in micrograms per liter or nanograms per milliliter, and detection limits vary, which is why cross-lab comparisons can mislead.
What the number represents
The number reflects the amount of BPA your body eliminated into urine during a brief window. Total BPA captures the integrated dose after your liver processed it. Free BPA, when reported, skews toward very recent or dermal exposure. Creatinine-corrected values (for example, micrograms per gram creatinine) help normalize for urine concentration and make repeat testing more comparable. High today, lower tomorrow? That’s common with nonpersistent chemicals.
What the Results Mean
Reference intervals vs. personal context
Population reference ranges show what’s common, not what’s “safe.” Large biomonitoring efforts, like CDC surveys, consistently find BPA in most people. Interpretation shifts with age, pregnancy, kidney function, hydration, and even shift-work patterns that influence when you eat and what you touch. Lab methodology also matters: total vs free BPA, detection limits, and whether creatinine correction is used can change the picture. Your number is a clue, not a verdict.
Pattern recognition
Spikes can tell a story. A disproportionately high free BPA with a same-day collection sometimes points toward recent dermal contact, such as handling thermal receipts at work. A higher total BPA on a day heavy in canned or packaged foods suggests ingestion as the main route. Seeing BPA analogues like BPS or BPF elevated alongside BPA can hint that “BPA-free” replacements are in the mix. No single pattern is definitive, but clusters often map to real habits.
Follow-up testing
Because BPA clears quickly, retesting after adjusting suspected exposures can help confirm what matters most. Use the same lab, sample type, and dilution correction strategy, ideally at the same time of day. Capturing both a weekday and a weekend can reveal occupational versus dietary patterns. Watch trend lines. A sustained downward shift usually tells you you’re reading the right signals.
Key Systems Affected
Nervous system
BPA interacts with estrogen and thyroid signaling—pathways the brain uses for development and function. Research links prenatal and early-life exposure to neurodevelopmental differences in some cohorts, though findings are not uniform. In adults, studies explore associations with mood and cognition, but causality is not established. Mechanistically, BPA can bind estrogen receptors and modulate gene expression that shapes synaptic wiring. Translation: subtle signals can matter, especially during fetal and infant windows.
Liver and detox pathways
The liver is the metabolic hub for BPA. Enzymes tag BPA with glucuronic acid or sulfate to render it water-soluble, then it exits via urine. This phase II chemistry leans on carbohydrate metabolism and sulfur pools. Oxidative stress markers can rise with higher exposures in some studies, and liver enzymes like ALT and GGT sometimes track with phenol mixtures. But individual labs aren’t diagnostic—context with other markers and clinical history is key.
Kidneys and filtration
Kidneys handle the final step: excretion. Reduced kidney function can alter measured urinary levels and complicate dilution correction. That’s why creatinine-corrected results and, when needed, specific gravity are helpful for interpretation. Hydration state affects raw concentrations. If renal function is impaired, the same exposure may yield different numbers, making trend tracking even more important.
Endocrine and metabolism
BPA is an endocrine-active compound. It can mimic or modulate estrogen signaling, interact with androgen pathways, and influence thyroid hormone dynamics. Observational studies have linked higher BPA levels with insulin resistance patterns and certain reproductive findings, including in conditions like PCOS, though mechanisms are still under investigation. The body’s receptors are like lock-and-key systems; BPA can be a pick that jostles the door without fully opening it.
Common Sources of Exposure
Environmental and household
Thermal paper receipts are a notable non-dietary source—BPA can transfer to skin on contact. Epoxy resins used in some can linings and older polycarbonate plastics are classic contributors. Indoor dust can carry trace amounts from consumer products. Some dental materials historically contained BPA derivatives, though many formulations have shifted. Homes that feel “green” on the surface can still house micro-sources you wouldn’t intuitively flag.
Dietary and occupational
Canned soups, beans, and sodas, plus certain jar lids and takeout packaging, have historically been frequent sources. Heating contents in contact with plastics can increase migration. Occupations with routine receipt handling—think cashiers—often show distinct exposure profiles in studies. Industrial settings using epoxy resins may also elevate risk. The route matters because ingestion and dermal contact can look different in timing and magnitude.
Clues from history
Notice a pattern after a stretch of convenience foods during travel? Handling a thick stack of receipts during holiday retail hours? Recently switched to “BPA-free” products and now seeing BPS or BPF on your report? Even small routine changes can shift exposure. Your calendar can be as informative as your lab slip—what changed in the 24–48 hours before your test?
Detoxification and Elimination
Physiology 101
BPA is mostly metabolized via glucuronidation and sulfation in the liver, then eliminated through urine. The half-life is short—on the order of hours—so levels reflect recent intake or contact. There may be some enterohepatic recirculation, where conjugated BPA gets deconjugated in the gut and briefly reabsorbed. Nonetheless, for most people, the system acts like a quick-pass filter that resets rapidly when exposure dips.
Systems that support clearance
Phase II enzymes attach glucuronic acid or sulfate, transporters shuttle conjugates into bile and urine, and kidneys finalize removal. Microbiome enzymes can influence deconjugation in the gut. Adequate liver blood flow, renal perfusion, and intact transport mechanisms all affect how swiftly BPA exits. It’s a relay race—if one runner slows, the baton lingers.
Why responses vary
Genetic differences in glucuronidation and sulfation enzymes, nutrient status related to sulfur amino acids, age, pregnancy, co-exposures to BPA analogues, and acute illness can all shift elimination rates. Children often show different patterns than adults. Hydration and activity level change urine concentration independent of exposure. Two people, same environment, not always the same number—biology personalizes the printout.
Biomarker Correlations
Functional context from broader labs
Pairing a BPA result with broader panels can connect exposure to physiological patterns. Thyroid tests (TSH, free T4), metabolic markers (fasting glucose, insulin), lipid profiles, and liver enzymes (ALT, GGT) create a more complete map. Inflammation signals like hs-CRP and oxidative stress markers add color, though associations with BPA are mixed across studies. Urinary creatinine and specific gravity anchor interpretation by correcting dilution.
Nutrient cofactors and capacity
Glucuronidation uses UDP-glucuronic acid generated from glucose metabolism, while sulfation draws on sulfate derived from methionine and cysteine. Selenium and iodine status support thyroid resilience, which is relevant when assessing endocrine-active exposures. Antioxidant capacity—shaped by glutathione and related systems—modulates redox balance when phenols and other stressors stack up. It’s systems biology, not a single switch.
Interpreting together
Rising total BPA alongside a normal thyroid panel may reflect exposure without an observable endocrine effect—at least at that point in time. A spike in free BPA the same day you handled receipts gives a timing clue that points to dermal contact. Stable creatinine-corrected BPA with shifting raw concentrations often indicates hydration changes more than true exposure shifts. Seeing BPS or BPF trend upward while BPA decreases suggests product substitution rather than elimination of exposure.
Optimal vs. Normal
Population ranges
Reference ranges show where most people land today. They are not health-based targets. National surveys report detectable BPA in a majority of urine samples, reflecting how common exposure is in modern life. Because methods differ across labs and studies, stay consistent with one approach when tracking over time. Comparisons to published percentiles can be helpful orientation, not a diagnosis.
Longevity-oriented targets
Many clinicians consider “as low as reasonably achievable” a practical aim for nonpersistent environmental chemicals. That doesn’t mean zero is always feasible or necessary. It means using your baseline to judge whether exposures are routine background or unusually high for you. The focus is on pattern recognition and reduction of avoidable spikes rather than chasing an arbitrary cutoff.
Trend over time
Direction often matters more than a single value. If your creatinine-corrected BPA trends downward across similar testing conditions, your changes are probably aligning with reality. Travel, seasonal eating shifts, and job demands can create temporary highs that settle when routines stabilize. Track with intention. Short half-life chemicals reward timely retesting to validate the story.
Why Testing Is Worth It
From mystery to measurement
BPA testing turns a vague idea—“I think I’m exposed”—into a number you can contextualize. Large biomonitoring data sets show that exposure is common. Your test tells you whether your recent window looks typical for the population or suggests standout sources. It’s the difference between guessing and having a dashboard.
Guiding remediation
Results help you prioritize. A profile leaning toward very recent dermal exposure points attention toward handling practices and timing. A pattern that tracks with food choices suggests packaging contact as the main route. When analogues like BPS show up alongside BPA, the signal shifts toward product substitutions that matter. The test helps you decide which lever is worth pulling first.
Prevention and baseline
A personal baseline creates a reference you can revisit after travel, job changes, or new kitchen habits. Because BPA clears quickly, you can see whether adjustments translate into measurable differences within weeks. Over time, your data becomes a map of what really moves the needle for you, not just what should on paper.
From Lab Values to Next Steps with Superpower
Environmental exposure is measurable and meaningful when you connect it to how your body responds. BPA testing shows recent contact; broader physiology shows how resilient your system looks in the same window. Put those together and patterns stop being mysterious—they become manageable.
Want the full picture? Pair targeted BPA testing with Superpower’s 100+ biomarker panel to see exposure, hormone balance, liver function, glucose control, inflammation, and more in one view.