Key Benefits
- Check vitamin D status and calcium balance to protect bones and muscles.
- Spot low vitamin D early, before fractures or muscle weakness develop.
- Clarify cramps, bone aches, or tingling possibly linked to low calcium or D.
- Guide safe supplement dosing and sunlight habits to reach target levels.
- Support pregnancy by ensuring levels needed for fetal bones and maternal health.
- Track seasonal shifts and treatment response to keep levels steady year‑round.
- Flag abnormal calcium that can signal severe deficiency or parathyroid issues.
- Best interpreted with parathyroid hormone, phosphorus, and your symptoms.
What are Vitamin D Deficiency
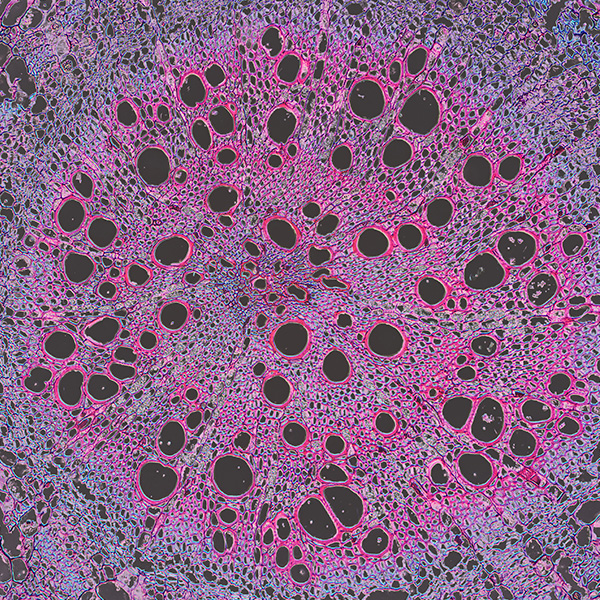
Vitamin D deficiency biomarkers show whether your body has enough vitamin D to keep calcium balanced, build strong bones, support muscles, and regulate immune signaling. The core marker is 25-hydroxyvitamin D (25[OH]D, calcidiol), the storage form made in the liver from vitamin D you make in skin or get from food; it reflects your overall vitamin D supply over time. Your body’s hormonal response is tracked with parathyroid hormone (PTH), which rises when vitamin D is low to defend blood calcium, signaling strain on bone and mineral balance. The active hormone 1,25-dihydroxyvitamin D (calcitriol) is produced in the kidney and drives calcium absorption; it shows activation status but does not reliably indicate vitamin D stores. Downstream effects appear in minerals and bone enzymes, including calcium, phosphate, and alkaline phosphatase (ALP), which shift as bone turnover increases in deficiency. Taken together, these biomarkers map intake, storage, activation, and impact, enabling precise detection of deficiency and its physiological consequences.
Why are Vitamin D Deficiency biomarkers important?
Vitamin D deficiency biomarkers tell you how well your body maintains the calcium–bone–muscle axis while influencing immune and hormone signaling. The key marker is 25‑hydroxyvitamin D, which reflects vitamin D stores; calcium shows whether the system is staying in balance; parathyroid hormone (PTH) often shifts in response to both.
Many labs consider 25‑hydroxyvitamin D deficient below 20, borderline 20–29, and generally adequate around 30–50, with optimal values often in the middle to upper part of that adequate band. Serum calcium usually sits about 8.5–10.2, and the healthiest physiology tends to cluster near the middle of this range.
When 25‑hydroxyvitamin D runs low, the gut absorbs less calcium, PTH rises (secondary hyperparathyroidism), and calcium is mobilized from bone. People may notice bone aching, muscle weakness, cramps, or fatigue; children can develop rickets and delayed growth, teens may miss peak bone mass, adults can develop osteomalacia and higher fracture risk, and older adults face more falls. During pregnancy, low vitamin D is linked to suboptimal fetal skeletal mineralization and maternal bone strain.
Very high 25‑hydroxyvitamin D is uncommon but can drive hypercalcemia, bringing nausea, constipation, confusion, arrhythmias, or kidney stones; calcium values above the usual range may point to disorders such as primary hyperparathyroidism.
Big picture, these biomarkers sit at the crossroads of bone remodeling, kidney and liver activation steps, PTH feedback, muscle performance, and immune tone. Persistently low vitamin D signals stress across this network, increasing risks for osteoporosis and fractures and associating with adverse cardiometabolic and infection outcomes over time.
What Insights Will I Get?
Vitamin D deficiency testing matters because it sits at the center of mineral metabolism that stabilizes bones, muscles, nerves, and immune tone. Through calcium–phosphate balance, it influences energy use, neuromuscular control, cardiovascular resilience, and aspects of cognition. At Superpower, we test these biomarkers: Vitamin D and Calcium.
Vitamin D testing refers to 25-hydroxyvitamin D, the main circulating reservoir that best reflects body stores. It enables intestinal calcium absorption and shapes parathyroid hormone activity. Calcium is measured in blood (typically total calcium) and is tightly regulated—the visible outcome of the vitamin D–parathyroid–kidney–bone network.
What this means for stability and healthy function: Adequate Vitamin D supports efficient calcium handling, balanced bone remodeling, reliable muscle contraction, and well-calibrated immune signaling. Low Vitamin D signals reduced calcium absorption and a shift toward secondary hyperparathyroidism with higher bone resorption; overt symptoms usually appear later. Calcium helps stage this process. Normal calcium can persist despite deficiency due to hormonal compensation. Low calcium suggests decompensation or coexisting renal, endocrine, or malabsorption issues. High calcium typically points away from vitamin D deficiency and toward other causes of mineral dysregulation.
Notes: Interpretation varies with season, latitude, skin pigmentation, age, and pregnancy. Chronic kidney or liver disease, malabsorption, obesity, and medications such as anticonvulsants or glucocorticoids can shift levels. Assay methods differ across labs. Total calcium is influenced by albumin; ionized calcium more directly reflects biologically active calcium, especially in acute illness.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


