Key Benefits
- Check bone-building nutrients and calcium balance to reduce osteoporosis and fracture risk.
- Spot low vitamin D that limits calcium absorption and weakens bone mineralization.
- Clarify muscle cramps, bone pain, tingling, or fatigue tied to calcium imbalance.
- Guide safe vitamin D and calcium supplementation and osteoporosis therapy planning.
- Flag possible parathyroid or kidney issues when corrected calcium is high or low.
- Clarify nutrition and inflammation status with albumin, ensuring accurate corrected calcium interpretation.
- Track progress by trending vitamin D and corrected calcium during treatment or lifestyle changes.
- Best interpreted with PTH, kidney function, phosphorus, and bone density alongside your symptoms.
What are Osteoporosis
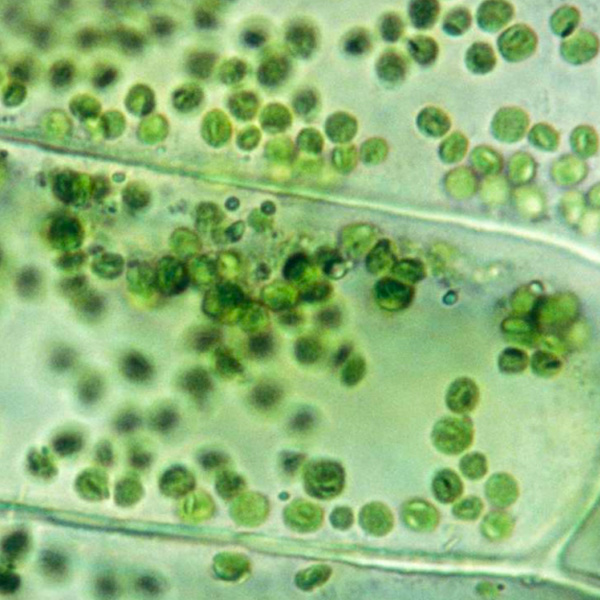
Osteoporosis biomarkers are blood and urine signals that capture how fast your skeleton is being broken down and rebuilt—the ongoing remodeling that keeps bone strong. They come from bone tissue or from the hormones that control calcium–bone metabolism. When bone is being resorbed, tiny fragments of type I collagen enter circulation (CTX, NTX). When bone is being formed, precursor pieces and enzymes appear (P1NP, bone-specific alkaline phosphatase), along with osteocalcin. Together these markers show the pace and tilt of remodeling (resorption vs formation). Testing provides a dynamic view that a bone density scan cannot: it can show current activity, help tailor therapy choice and dose, and confirm biological response within weeks to months. Regulators such as parathyroid hormone (PTH) and vitamin D (25-hydroxyvitamin D) add context by indicating how the calcium–bone axis is being signaled. By translating the invisible churn of bone into measurable signals, these biomarkers make osteoporosis less of a waiting game—enabling earlier action, more personalized care, and ongoing monitoring of how well the skeleton is being protected.
Why are Osteoporosis biomarkers important?
Osteoporosis biomarkers are the blood signals that tell us how the body is managing bone turnover and calcium economy. Vitamin D reflects intestinal calcium absorption; calcium shows the circulating mineral available for bone and neuromuscular function; albumin carries calcium in the blood; corrected calcium estimates the true calcium level by accounting for albumin. Together, they reveal how bone, parathyroid glands, kidneys, gut, and muscles are coordinating mineral balance.
Typical reference ranges: Vitamin D is generally sufficient around 30–50, with most people healthiest in the middle. Total calcium usually sits near 8.5–10.2, and stability in the middle is reassuring. Albumin is commonly 3.5–5.0; corrected calcium should align with the same tight mid-range as total calcium when albumin is normal. Values drifting high can signal over-supplementation, hyperparathyroidism, or dehydration; very high calcium may cause constipation, kidney stones, confusion, and can accelerate bone loss by increasing bone resorption.
When values run low, physiology compensates in bone-harming ways. Low Vitamin D (often below 20) reduces calcium absorption, triggers secondary hyperparathyroidism, and accelerates trabecular bone loss—felt as bone pain, muscle weakness, cramps, and higher fall and fracture risk. Low calcium can cause tingling, spasms, or arrhythmias while pulling calcium from bone. Low albumin makes total calcium appear low even when ionized calcium is normal; corrected calcium clarifies this. Postmenopausal women lose bone faster under these stresses; children may show delayed growth or rickets; in pregnancy, albumin naturally falls, making correction essential.
Big picture: these biomarkers integrate bone with endocrine, renal, and gastrointestinal systems. Keeping them in a steady mid-range supports strong skeletons, steadier gait and muscle function, and lowers the lifetime risks of fragility fractures, pain, and loss of independence.
What Insights Will I Get?
Bone is a dynamic endocrine organ. Its mineral balance influences muscles, nerves, heart rhythm, immunity, and overall metabolism through calcium and hormone signaling. Osteoporosis reflects chronically imbalanced remodeling. At Superpower, we test these specific biomarkers: Vitamin D, Calcium, Albumin, Corrected Calcium.
Vitamin D is a steroid prohormone (25‑hydroxyvitamin D in most labs) that enables intestinal calcium absorption and restrains parathyroid hormone (PTH). Low Vitamin D drives secondary hyperparathyroidism, higher bone turnover, and loss of mineral density. Adequate levels support stable calcium balance and resilient bone matrix.
Calcium in blood is tightly regulated and mirrors the calcium–PTH–vitamin D axis more than dietary intake. High or low values can signal disorders that accelerate bone resorption or impair mineralization. A stable normal calcium suggests balanced remodeling; sustained deviations indicate system instability.
Albumin is the main plasma protein that binds calcium and reflects inflammatory and nutritional status. Low albumin lowers measured total calcium even when the physiologically active fraction is unchanged. It contextualizes calcium results and signals systemic stressors linked to bone fragility.
Corrected Calcium estimates what total calcium would be if albumin were normal, better approximating ionized (bioactive) calcium. It helps distinguish true calcium imbalance from low albumin effects, clarifying parathyroid–vitamin D dynamics relevant to osteoporosis risk.
Notes: Interpretation varies with age, menopause status, pregnancy, kidney or liver disease, acute illness, and hydration. Medications (e.g., glucocorticoids, anticonvulsants, thiazides, lithium) and assay variability affect results. Vitamin D fluctuates with season, sun exposure, and skin pigmentation.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


