Key Benefits
'- Screen for soft bones (osteomalacia) using vitamin D, calcium, and ALP results.
- Spot vitamin D deficiency that weakens bone mineralization and increases fracture risk.
- Flag low or borderline calcium that signals impaired mineralization and bone pain.
- Identify raised ALP that points to active bone repair from osteomalacia.
- Explain muscle weakness, waddling gait, or diffuse aches by linking labs to bone softening.
- Guide targeted vitamin D and calcium replacement to restore mineralization and relieve symptoms.
- Track recovery with rising vitamin D, steady calcium, and falling ALP over time.
- Best interpreted alongside phosphate, parathyroid hormone, and your symptoms for accuracy.
What are Osteomalacia
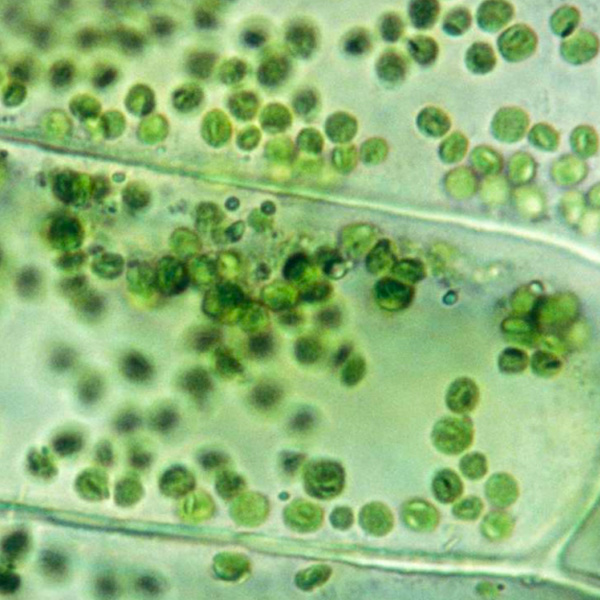
Osteomalacia biomarkers are blood and urine signals that show whether your bones are being properly hardened with minerals. They track the body’s mineral supply (calcium and phosphate), the nutrient that enables absorption and mineral delivery (vitamin D), the hormones that regulate this system, and the activity of bone‑forming cells. Core markers include vitamin D storage status (25‑hydroxyvitamin D), the active vitamin D hormone (1,25‑dihydroxyvitamin D), circulating calcium and phosphate, the calcium‑regulating hormone from the neck glands (parathyroid hormone, PTH), and the enzyme released when new bone is laid down (alkaline phosphatase, especially bone‑specific ALP). Some panels also measure the phosphate‑controlling signal made by bone (fibroblast growth factor 23, FGF23) and proteins that reflect bone turnover (osteocalcin, P1NP, CTX). Together, these tests reveal where the mineralization pathway is faltering—insufficient vitamin D input, phosphate loss, or disrupted handling in the gut or kidneys—and distinguish soft, under‑mineralized bone from other bone conditions. In short, they pinpoint the biological bottleneck so treatment can target the cause, not just the symptoms.
Why are Osteomalacia biomarkers important?
Osteomalacia biomarkers tell you how well your skeleton is being mineralized—and how the gut, kidneys, parathyroid glands, and muscles are coordinating to keep calcium and phosphate where they belong. They flag when bone is built but left “soft,” leading to pain, weakness, and fractures.
Vitamin D is typically considered sufficient around 30–50, with most people doing best in the middle of that range. Serum calcium commonly sits near 8.5–10.2, where a steady middle value supports nerve and muscle function. Alkaline phosphatase (ALP) in adults is often about 40–120, and healthy states tend to fall on the low-to-middle end; sustained elevations suggest increased bone turnover.
When vitamin D is low, intestinal calcium absorption drops. Calcium may be low or low–normal, the parathyroid glands ramp up (secondary hyperparathyroidism), and bone matrix fails to mineralize. ALP usually rises as osteoblasts work overtime. People feel deep, aching bone pain (hips, ribs, pelvis), thigh and shoulder-girdle weakness, difficulty climbing stairs, a waddling gait, and stress or fragility fractures. Men and women are both affected; risk increases with aging and in postmenopausal women. In children and teens, the same physiology appears as rickets—growth plate pain, bowed legs, and delayed motor milestones. During pregnancy, higher mineral demands can unmask deficiency, with cramps, tingling, or bone pain.
Big picture, these markers integrate sunlight and diet (vitamin D), liver–kidney activation pathways, parathyroid control, and skeletal remodeling. Keeping them in balance supports mobility, neuromuscular stability, and fracture resistance—key to independence and long-term quality of life.
What Insights Will I Get?
Osteomalacia reflects impaired bone mineralization, which can reverberate through muscle strength, nerve conduction, and whole‑body calcium–phosphate balance. Tracking its core biomarkers helps map that physiology in real time. At Superpower, we test Vitamin D, Calcium, and Alkaline Phosphatase (ALP). Together they show how effectively you absorb, mobilize, and mineralize the building blocks of bone.
Vitamin D (measured as 25‑hydroxyvitamin D) is the prohormone that enables intestinal absorption of calcium and phosphate; deficiency drives secondary hyperparathyroidism and unmineralized osteoid—hallmarks of osteomalacia. Serum Calcium reflects the immediate extracellular pool; it may be low or maintained at the expense of bone. ALP, largely from osteoblasts, rises when bone turnover accelerates in response to defective mineralization.
Healthy Vitamin D status signals an intact endocrine axis and efficient mineral supply to the skeleton, supporting neuromuscular stability and immune modulation. Stable Calcium within reference indicates balanced bone buffering and reliable cardiac and nerve function; low or labile values suggest strained homeostasis. A normal ALP fits steady remodeling; a high ALP with low Vitamin D points to high‑turnover, under‑mineralized bone.
Interpretation varies with age (higher ALP in growth), pregnancy, and lactation. Kidney or liver disease alters vitamin D activation and mineral balance. Anticonvulsants, glucocorticoids, and antiretrovirals affect vitamin D metabolism. Seasonal sun exposure and skin pigmentation influence vitamin D levels. Assay methods and lab reference ranges differ.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


