Key Benefits
- Understand overall heart attack risk from inflammation and cholesterol balance.
- Spot hidden artery inflammation; higher hs-CRP links to higher myocardial infarction risk.
- Flag atherogenic cholesterol; high LDL and low HDL increase plaque buildup risk.
- Clarify risk when cholesterol looks “okay”; elevated hs-CRP can still warn.
- Guide statin and lifestyle intensity when risk is borderline or intermediate.
- Track treatment impact; falling LDL and hs-CRP suggest lower future event risk.
- Avoid misdiagnosis; these tests cannot confirm an active heart attack.
- Best interpreted with other risk factors and a 10-year heart risk calculator.
What are Myocardial Infarction
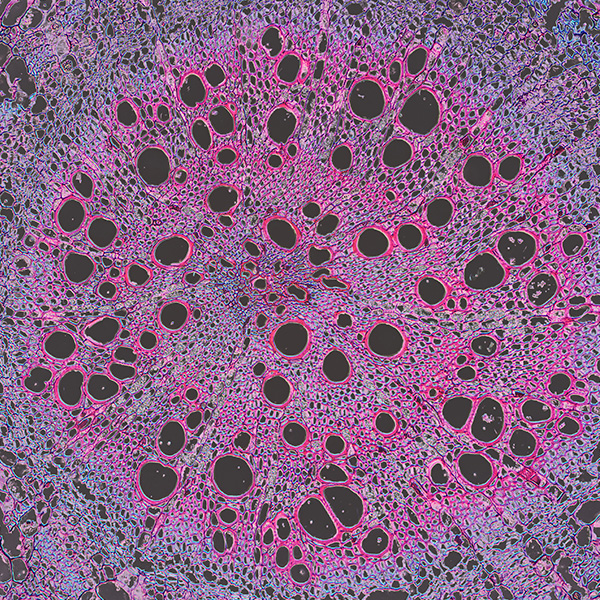
Myocardial infarction biomarkers are measurable signals in the blood that appear when heart muscle is injured by a blocked artery. In a heart attack, a section of heart loses oxygen, cells run out of energy, and their membranes break down. This releases internal proteins from heart muscle cells (cardiomyocytes) into the circulation, creating a biological “trace” of damage that clinicians can detect and track over time. The key markers are cardiac troponins—regulatory proteins from the contractile machinery that control heartbeat force (cardiac troponin I and T, cTnI/cTnT). Because they are specific to heart muscle and rise and fall in a characteristic time pattern, they anchor the diagnosis and timing of injury. Older or adjunct markers include an energy enzyme (creatine kinase-MB, CK-MB) and an oxygen-binding protein (myoglobin), which can appear earlier but are less specific to the heart. Together, these biomarkers translate cell-level damage into clear evidence in the blood, enabling rapid confirmation of a heart attack and prioritizing urgent care.
Why are Myocardial Infarction biomarkers important?
Myocardial infarction biomarkers are blood signals of heart muscle stress, injury, and the vascular/inflammatory forces that cause it. High-sensitivity cardiac troponins show actual heart cell damage, while hs-CRP and LDL/HDL reflect the inflammability and cholesterol traffic that build or stabilize plaques across arteries, affecting heart, brain, and kidneys.
In practice, a troponin value below the assay’s 99th-percentile cutoff is typical and reassures against ongoing necrosis. For hs-CRP, the low range aligns with lower cardiovascular risk, mid-range is average, and high indicates greater risk. LDL is safer toward the low end; HDL is more protective toward the high end.
When values sit low—undetectable troponin, low hs-CRP, low LDL with higher HDL—they reflect quiet inflammation, fewer vulnerable plaques, and no active cell death. Symptoms are often absent or limited to exertional tightness if fixed narrowing exists. Women have lower troponin thresholds; children rarely show MI patterns; in pregnancy, HDL tends to rise.
High troponin signals myocardial cell rupture and enzyme leak, often with chest pressure, shortness of breath, sweating, palpitations, or sudden fatigue; complications include arrhythmias and pump failure. High hs-CRP suggests active vascular inflammation, and higher LDL with low HDL tracks with unstable plaque burden. Typical mid-range values map to average population risk.
Together, these markers connect biology to prognosis: they link liver lipid handling, immune tone, endothelial health, and kidney clearance to the heart’s oxygen supply. Trended over time, they help gauge plaque activity and injury risk, informing the likelihood of future infarction, heart failure, and stroke.
What Insights Will I Get?
Myocardial infarction (heart attack) reflects the failure of coronary blood flow to meet the heart’s energy demand. Biomarkers that track arterial inflammation and lipoprotein balance reveal how resilient your cardiovascular system is—how well it can deliver oxygen for metabolism, protect cognition through stable perfusion, and support whole‑body function. At Superpower, we test high‑sensitivity C‑reactive protein (hs‑CRP) and LDL/HDL markers.
hs‑CRP is a liver protein that rises with low‑grade systemic and vascular inflammation. In the coronary arteries, higher hs‑CRP signals active inflammatory biology around plaques. LDL and HDL are lipoproteins: LDL delivers cholesterol into tissues and arterial walls, promoting plaque formation (atherogenesis), while HDL participates in reverse cholesterol transport, helping clear cholesterol from arteries. Their balance shapes plaque growth and the likelihood of rupture and thrombosis—the immediate trigger for myocardial infarction.
When hs‑CRP is near the low end of its reference range, it suggests a quieter endothelium and more stable plaques; higher values imply endothelial activation, oxidative stress, and greater plaque vulnerability. A favorable LDL/HDL pattern indicates lower atherogenic burden and more efficient cholesterol efflux, supporting stable coronary flow and steady cardiac energy supply. An unfavorable pattern (higher LDL and/or lower HDL) points to increased lipid deposition, foam cell formation, and impaired repair capacity.
Notes: hs‑CRP rises transiently with infection, injury, surgery, and vigorous exercise; interpret away from acute illness. Lipids vary with age, genetics, pregnancy, weight changes, and medications (e.g., statins, PCSK9 inhibitors, estrogens). Fasting status has modest impact on LDL/HDL. Use high‑sensitivity assays for CRP and consider lab‑to‑lab variability when trending results.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


