Key Benefits
- Spot low potassium early to protect muscle function and heart rhythm.
- Clarify symptoms like weakness, cramps, constipation, or palpitations linked to low potassium.
- Flag medication effects from diuretics, laxatives, or insulin that lower potassium.
- Guide treatment by adjusting potassium supplements and correcting low magnesium.
- Reduce arrhythmia risk if you have heart disease or take digoxin.
- Support pregnancy care when severe vomiting or dehydration triggers low potassium.
- Track trends during illness or recovery to prevent recurrent low levels.
- Best interpreted with magnesium, bicarbonate, urine potassium, kidney function, and your symptoms.
What are Hypokalemia
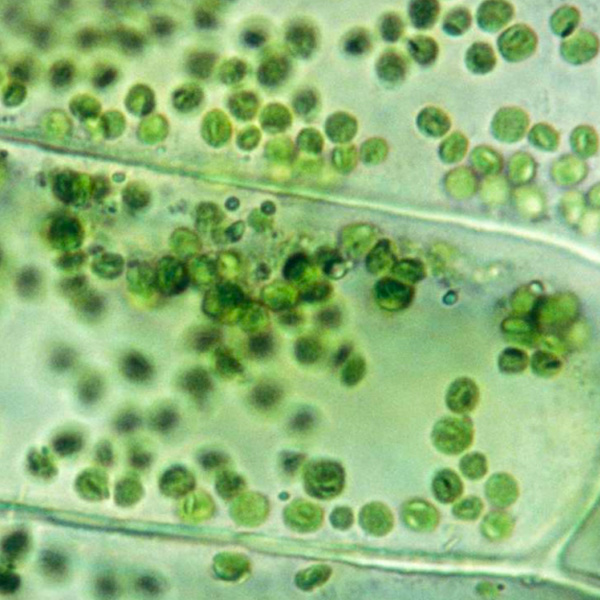
Hypokalemia biomarkers are lab signals that show how much potassium your body has available and why it’s been depleted. The core measure is blood potassium (serum K+), which reflects the ion that sets the electrical resting state of nerves and muscles (membrane potential) and stabilizes heart rhythm (cardiac electrophysiology). Surrounding biomarkers help explain the cause: acid–base balance markers (bicarbonate, pH) point to losses or shifts; kidney electrolytes and hormones (urinary potassium and chloride, renin, aldosterone) indicate whether the kidneys are wasting potassium or responding to hormone drive (renin–angiotensin–aldosterone system). Magnesium level (Mg2+) matters because deficiency promotes ongoing potassium loss. Blood glucose and stress signals (insulin, catecholamines) can shift potassium into cells (transcellular shift), and kidney function markers (creatinine, eGFR) show how well the kidneys can conserve it. Together, these biomarkers move you from simply spotting a problem to pinpointing its source, guiding safe replacement and addressing the root cause to protect muscles and the heart from weakness, cramps, and dangerous rhythm disturbances.
Why are Hypokalemia biomarkers important?
Hypokalemia biomarkers tell us when body potassium is too low. Potassium sets the electrical resting state of nerves and muscles, so even small deficits can reverberate through the heart’s rhythm, skeletal and smooth muscle function, kidney water balance, and insulin signaling.
The cornerstone test is blood potassium. Typical reference range is about 3.5–5.0, and the physiologic sweet spot tends to be mid‑range, often in the low‑to‑mid 4s. Urine potassium, acid–base status, and magnesium help distinguish renal from gastrointestinal losses and shifts of potassium into cells.
When values fall below range, the body is usually losing potassium (diuretics, vomiting/diarrhea, excess aldosterone) or driving it into cells (alkalosis, insulin surges, certain medications). Nerve and muscle cells become hyperpolarized, leading to fatigue, muscle cramps, weakness, constipation or ileus, and, if severe, flaccid paralysis. The heart becomes electrically irritable, with palpitations and risk of dangerous arrhythmias. Kidneys may lose concentrating ability, causing thirst and frequent urination, and metabolic alkalosis can emerge. Older adults and people with heart disease or on diuretics are especially vulnerable to rhythm disturbances. Pregnancy with significant vomiting increases risk. Low magnesium often coexists and magnifies these effects.
Big picture: potassium status integrates kidney handling, mineralocorticoid hormones (aldosterone), acid–base balance, and glucose–insulin dynamics. Tracking hypokalemia biomarkers helps uncover causes such as primary aldosteronism or renal tubular losses and signals risks that span exercise tolerance, blood pressure control, arrhythmias, and long‑term cardiovascular outcomes.
What Insights Will I Get?
Potassium status is fundamental to electrical signaling, muscle contraction, vascular tone, acid–base balance, and kidney concentrating ability. Low blood potassium—hypokalemia—can destabilize heartbeat, reduce neuromuscular performance, and alter glucose handling. At Superpower, we test these specific biomarkers: Potassium.
Potassium is the major intracellular cation; only a small fraction circulates in blood and is regulated by the kidneys and hormones (insulin, catecholamines, aldosterone). Hypokalemia means the blood level is below the usual reference interval; it reflects either a true total-body deficit or a shift of potassium from blood into cells.
A low potassium signals reduced electrical stability of heart and nerves, higher arrhythmia susceptibility, muscle weakness or cramps, and constipation, with decreased insulin secretion and transient glucose intolerance. It also indicates stress on renal tubular function (impaired urine concentration, metabolic alkalosis). Stable, mid‑range potassium suggests resilient homeostasis across these systems.
Notes: Interpretation depends on context. Alkalosis, insulin, beta‑agonists, and catecholamine surges drive potassium into cells; gastrointestinal or renal losses (diuretics, laxatives, corticosteroids, amphotericin) reduce body stores; hyperaldosteronism and Cushing syndrome physiology promote renal wasting; low magnesium perpetuates hypokalemia. Pregnancy, age, kidney function, and sample handling (serum vs plasma, delays, hemolysis causing pseudohyperkalemia) affect results. Reference limits vary by method and population.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


