Key Benefits
- Check potassium to detect and confirm dangerous high levels that can harm the heart.
- Spot early imbalance from kidney disease, diabetes, or adrenal problems before symptoms.
- Flag medication effects from ACE inhibitors, ARBs, NSAIDs, or potassium-sparing diuretics.
- Clarify causes of weakness, numbness, or palpitations by linking them to potassium.
- Guide urgency and treatment steps when levels are critical to prevent dangerous rhythms.
- Track trends during chronic kidney disease, heart failure, or dialysis care.
- Confirm true elevation by repeating tests and avoiding sample problems that raise potassium.
- Best interpreted with creatinine, bicarbonate, glucose, and an EKG.
What are Hyperkalemia
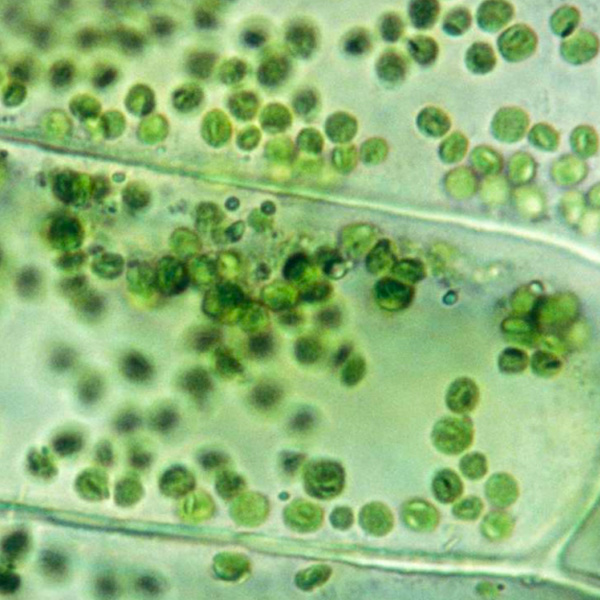
Hyperkalemia biomarkers are signals that show how much potassium is in the bloodstream and how the body is handling it. The primary marker is the measured potassium level in blood (serum K+), which confirms excess and reflects the balance between intake, cellular shifts, and kidney removal. Companion biomarkers map the “why.” Kidney filtration markers (creatinine, eGFR) indicate whether reduced excretion is contributing. Acid–base markers (bicarbonate, pH) show shifts that drive potassium out of or into cells. Hormones that govern salt and potassium balance (aldosterone, renin) reveal mineralocorticoid deficiency or resistance. Urinary measures of potassium excretion (urine K+) show whether the kidneys are wasting or retaining potassium. Markers of cell injury (creatine kinase) point to potassium release from damaged muscle. Finally, the heart’s electrical pattern (ECG) acts as a physiologic biomarker of potassium’s effect on membranes, signaling arrhythmia risk. Together, these tests do more than label “high potassium”—they locate the source of the problem and gauge its urgency so treatment can be targeted and timely.
Why are Hyperkalemia biomarkers important?
Hyperkalemia biomarkers—primarily the blood potassium test and, when severe, corroborating ECG changes—tell you how safely your cells can communicate. Potassium sets the electrical resting state of nerves and muscles, especially the heart. Even small shifts affect rhythm, muscle function, blood pressure control, and how kidneys and hormones maintain internal balance.
Most labs consider potassium roughly 3.5–5.0. For most people, the safest, “optimal” physiology sits near the middle of that range. Values below it reflect hypokalemia, not hyperkalemia, but they matter to the hyperkalemia story because both ends destabilize excitable tissues. Low potassium hyperpolarizes cell membranes, leading to fatigue, muscle cramps or weakness, constipation, and palpitations; the heart can develop ectopy or dangerous arrhythmias. It often accompanies losses from diuretics or vomiting, or high aldosterone states. Children and smaller adults may show symptoms sooner with rapid shifts; pregnancy usually maintains normal potassium, but vomiting-related losses can accentuate lows.
Values above range indicate true hyperkalemia or, less commonly, a sampling artifact. High potassium partially depolarizes cells, slowing conduction and risking peaked T waves, widened QRS, bradycardia, and ventricular arrhythmias, plus paresthesias and flaccid weakness. It most often reflects impaired renal excretion, low aldosterone activity, acidosis, tissue breakdown, or certain medications. Older adults and people with chronic kidney disease are particularly vulnerable.
Big picture: potassium sits at the crossroads of kidney function, adrenal-aldosterone signaling, acid–base status, insulin–glucose dynamics, and muscle integrity. Tracking it alongside creatinine, bicarbonate, and ECG findings links daily physiology to long-term outcomes, including arrhythmic risk, hospitalizations, and survival in kidney and cardiovascular disease.
What Insights Will I Get?
Hyperkalemia testing matters because potassium governs the electrical stability of every excitable tissue—heart, nerves, and muscles—and integrates with kidney function, acid–base balance, and hormonal control (renin–angiotensin–aldosterone). Disturbances ripple across cardiovascular rhythm, muscular performance, autonomic tone, and overall metabolic resilience. At Superpower, we test these specific biomarkers: Potassium.
Potassium is the body’s main intracellular mineral (primary intracellular cation). The blood test reflects the small fraction circulating outside cells. Hyperkalemia means potassium in the blood is higher than expected. This can result from reduced renal excretion or low aldosterone activity, from shifts of potassium out of cells (acidemia, insulin deficiency, tissue breakdown), or from an increased external load.
For system stability, potassium must stay within a narrow range to maintain the resting membrane potential. When elevated, the electrochemical gradient shrinks, leading to partial depolarization. In the heart, this slows conduction and destabilizes rhythm (arrhythmogenic risk). In skeletal muscle and nerves, it impairs contractility and signal transmission, contributing to weakness or altered sensation. Persistent hyperkalemia also points to stressed renal tubular handling and RAAS signaling, and it interacts with acid–base status, affecting vascular tone and autonomic balance.
Notes: Interpretation is influenced by sample factors (hemolysis, prolonged tourniquet or fist clenching, serum vs plasma differences, high white cells or platelets causing pseudohyperkalemia), medications that reduce renal potassium excretion, and conditions such as kidney disease, diabetes, adrenal insufficiency, acidosis, or recent tissue injury. Age, pregnancy, and assay methods can subtly shift reference ranges; labs define “normal” differently.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


