Key Benefits
'- Know your cholesterol particle and inflammation profile to gauge coronary artery risk.
- Spot LDL and ApoB overload that drives plaque growth and artery narrowing.
- Flag inherited Lp(a) risk that standard cholesterol panels often miss.
- Detect vessel inflammation with hs-CRP to refine risk and treatment urgency.
- Clarify protective HDL and plaque-forming balance using NHR and AIP scores.
- Guide treatment intensity: lifestyle, statins, ezetimibe, or PCSK9 inhibitors when indicated.
- Track progress and remaining risk to keep LDL, ApoB, and inflammation on target.
- Understand results best with blood pressure, diabetes, smoking, family history, and symptoms.
What are Coronary Artery Disease
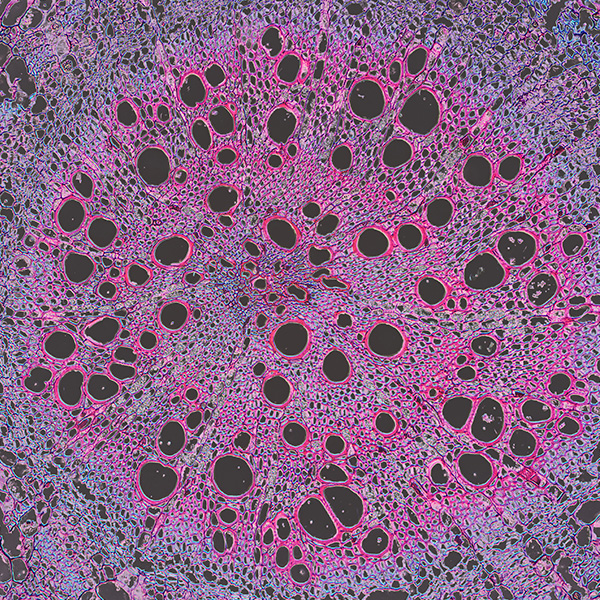
Coronary artery disease biomarkers are measurable signals in blood that mirror the formation, activity, and consequences of plaque in the heart’s arteries. They show how much artery-clogging cholesterol is in circulation (apoB‑containing lipoproteins such as LDL), whether the vessel wall is inflamed (high‑sensitivity C‑reactive protein), and whether the body is primed to form clots (fibrinogen, Lp[a]). They can also flag strain or injury to heart muscle when oxygen is limited (cardiac troponins; sometimes natriuretic peptides for wall stress). In addition, they capture metabolic states that accelerate plaque, like insulin resistance and disordered blood sugar (fasting glucose, HbA1c), alongside broader contributors. Taken together, these biomarkers translate hidden artery biology into actionable insight: estimating plaque burden, revealing silent or ongoing damage, guiding the intensity and type of prevention or treatment (lipid‑lowering, anti‑inflammatory, antithrombotic, lifestyle), and tracking response over time. In short, they let us “see” coronary disease early and manage it proactively, often long before symptoms or imaging make it obvious.
Why are Coronary Artery Disease biomarkers important?
Coronary artery disease biomarkers—LDL, HDL, ApoB, Lp(a), hs‑CRP, and ratios like NHR and AIP—trace how cholesterol traffic, genetics, and inflammation shape plaque in arteries, linking heart risk to metabolism, liver function, immunity, and clotting.
Across labs, LDL and ApoB are graded from desirable to high; lower is generally optimal. HDL protects more at the higher end. Lp(a) is ideally very low. hs‑CRP is best low, signaling quiet vascular inflammation. NHR and AIP are lowest—AIP often negative—when risk is lower. Women tend to have higher HDL; children usually have lower LDL/ApoB; pregnancy raises triglycerides, pushing AIP up and sometimes Lp(a).
When LDL and ApoB sit low, fewer atherogenic particles reach the artery wall and plaque growth slows; symptoms are uncommon. Low Lp(a) reduces calcific, clot‑prone plaque behavior. Low hs‑CRP, NHR, and AIP reflect calmer immune tone and larger, less dense lipoproteins, often tracking with insulin sensitivity.
At the high end, LDL/ApoB imply many cholesterol‑bearing particles and sustained plaque growth; elevated Lp(a), usually inherited, adds thrombosis and calcification. High hs‑CRP or NHR signals active vascular inflammation from infection, adiposity, or autoimmune disease. People may notice earlier angina or lower exercise tolerance—earlier in men, rising after menopause in women. Big picture: together these markers integrate lipid transport, genetics, and inflammation to forecast long‑term risks for heart attack, stroke, kidney disease, and heart failure.
What Insights Will I Get?
Coronary artery disease (CAD) biomarkers map how well your blood vessels deliver oxygen to the heart and, by extension, to the whole body’s energy system. They integrate lipid transport, inflammation, and clotting—processes that influence metabolism, cognition, resilience to stress, and immune balance. At Superpower, we test LDL, HDL, ApoB, Lp(a), hs-CRP, NHR, and AIP.
LDL carries cholesterol into artery walls; higher levels track with plaque formation. ApoB counts the total number of atherogenic particles (LDL and related remnants) that penetrate the endothelium. HDL supports reverse cholesterol transport and has antioxidant, anti-inflammatory actions. Lp(a) is a genetically set LDL-like particle with an attached apolipoprotein(a) that promotes plaque calcification and thrombosis. hs-CRP reflects systemic, vascular inflammation. NHR (neutrophil-to-HDL ratio) integrates innate immune activation with HDL functionality. AIP (log triglycerides/HDL) reflects small, dense LDL propensity and overall atherogenicity.
Together, these markers indicate plaque burden and stability. Lower ApoB and LDL signal fewer artery-penetrating particles; higher HDL suggests better cholesterol efflux and endothelial protection. Lower Lp(a) indicates reduced prothrombotic, pro-calcific drive. Lower hs-CRP and a favorable NHR point to quieter vascular inflammation. A lower AIP implies larger, less atherogenic lipoproteins and a more stable plaque phenotype—supporting steady coronary flow and myocardial energy supply.
Notes: Lipids rise with age, pregnancy, and some hormones; infections, trauma, and autoimmune flares elevate hs-CRP and NHR. Fasting status and recent exercise shift triglycerides and AIP. Lp(a) is largely genetic and stable. Medications and assay methods vary; interpret with repeat, context-aware testing.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


