Key Benefits
- Check how well your kidneys work and catch chronic kidney disease early.
- Stage CKD and track progression using creatinine and eGFR trends over time.
- Flag dehydration or high waste levels with BUN to explain fatigue or nausea.
- Clarify swelling and nutrition status by checking serum albumin for low levels.
- Protect heart rhythm by spotting dangerous potassium shifts from kidney decline or drugs.
- Protect bones and vessels by checking corrected calcium, adjusted for albumin levels.
- Guide safer meds, diet, fertility, and pregnancy planning based on kidney function.
- Best interpreted with urine albumin-to-creatinine ratio and your symptoms over time.
What are Chronic Kidney Disease
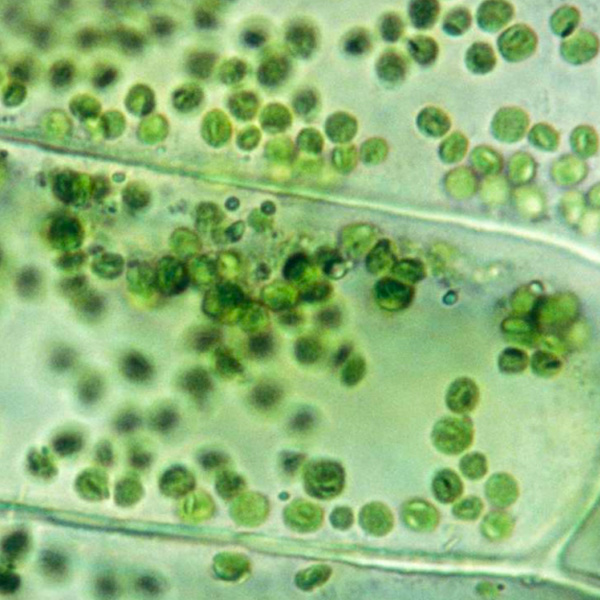
Chronic kidney disease biomarkers are measurable signals in blood and urine that reveal how well your kidneys filter waste, protect their delicate structures, and keep the body’s chemistry steady. They tell three main stories: filtration strength, leakiness, and whole‑body impact. Filtration markers (creatinine, cystatin C) show how efficiently the kidneys clear everyday waste and help estimate overall filtering capacity (glomerular filtration rate, GFR). Leak markers expose injury to the kidney’s filters and tubules—most simply as protein in the urine (albuminuria), and also via cellular stress signals from damaged tubule cells (NGAL, KIM‑1). Impact markers reflect the kidneys’ broader roles in salt–water balance and acid control (electrolytes, bicarbonate), mineral and bone regulation (phosphate, parathyroid hormone, PTH), and red blood cell support (erythropoietin, hemoglobin). Together, these biomarkers make a silent condition visible—enabling earlier detection, clearer staging, ongoing monitoring, and targeted therapy to protect kidney function and reduce cardiovascular risk.
Why are Chronic Kidney Disease biomarkers important?
Chronic Kidney Disease biomarkers are the body’s dashboard for kidney filtration, fluid–electrolyte balance, acid–base status, protein nutrition, and bone–mineral and heart–rhythm control. Together, creatinine, eGFR, BUN, albumin, corrected calcium, and potassium show how well the kidneys support every organ system.
Typical reference points: creatinine about 0.6–1.3 (lower in women and children); eGFR is best at or above 90 and stable; BUN about 7–20; albumin 3.5–5.0; corrected calcium 8.6–10.2; potassium 3.5–5.0. Optimal patterns tend toward a lower but stable creatinine for one’s muscle mass, an eGFR in the high-normal range, BUN mid-range, albumin in the upper-normal range, and calcium and potassium close to the middle. Rising creatinine or BUN suggests reduced filtration; low albumin flags inflammation or protein loss; calcium and potassium drifting off-center signal bone–mineral or electrical conduction risk.
When values run low, physiology shifts in specific ways. A low eGFR means fewer functioning nephrons, with fatigue, swelling, and reduced exercise tolerance; in children this can blunt growth. Low albumin promotes edema, weakness, and poor wound healing, and in CKD predicts worse outcomes. Low corrected calcium can cause tingling, cramps, or bone pain from secondary hyperparathyroidism. Low potassium brings muscle weakness and irregular heartbeats. Very low creatinine often reflects low muscle mass or pregnancy and can mask reduced kidney function when using creatinine-based estimates.
Big picture: these biomarkers knit kidneys to the heart, vessels, nerves, and skeleton. Their trajectories forecast cardiovascular events, arrhythmias, fractures, hospitalization, and survival, making them central to understanding disease stage, complications, and long-term risk.
What Insights Will I Get?
Kidneys are central to whole‑body stability: they clear metabolic waste, balance fluids and electrolytes, regulate acid–base status, activate hormones for blood pressure and bone health, and influence energy, cognition, and cardiovascular risk. Chronic kidney disease (CKD) disrupts these networks, so tracking filtration and homeostasis is key. At Superpower, we test Creatinine, eGFR, BUN, Albumin, Corrected Calcium, and Potassium.
Creatinine is a muscle‑derived waste cleared by glomerular filtration; higher blood levels suggest reduced filtration. eGFR estimates filtration capacity from creatinine and demographics, staging CKD severity. BUN reflects urea from protein metabolism; elevation indicates impaired clearance or altered nitrogen handling. Albumin is the main plasma protein; low serum levels can accompany kidney protein loss or inflammation. Corrected Calcium adjusts total calcium for albumin, reflecting bioactive calcium relevant to CKD‑mineral bone disorder. Potassium is a vital cation excreted by kidneys; CKD raises risk for abnormal levels.
Together, stable creatinine and eGFR indicate steady filtration; rising creatinine or falling eGFR signals declining function. BUN aligned with creatinine supports equilibrium, while disproportionate shifts hint at catabolic stress or volume changes. Adequate albumin supports oncotic pressure and vascular integrity. Normal corrected calcium suggests balanced mineral metabolism; deviation points to disordered bone–mineral regulation. Potassium within range supports electrical stability of the heart; extremes increase arrhythmia risk.
Notes: Interpretation varies with age, sex, muscle mass, and pregnancy (physiologic hyperfiltration). Acute illness, dehydration, and recent high protein intake affect BUN/creatinine. Medications (ACE inhibitors/ARBs, diuretics, NSAIDs) and assay variability influence values. Many labs now use race‑free eGFR equations.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


