Key Benefits
'- Gauge your artery-clogging risk by combining cholesterol, particle, and inflammation signals.
- Spot inherited Lp(a) risk that standard cholesterol misses, refining lifetime heart and stroke risk.
- Clarify hidden particle burden with ApoB, even when LDL appears normal.
- Flag active vascular inflammation with hs-CRP to reclassify borderline cardiovascular risk.
- Guide LDL goals and therapy intensity to slow plaque and prevent heart attacks, strokes.
- Track treatment response and lifestyle impact by trending LDL, ApoB, and hs-CRP.
- Add nuance with AIP and AC to flag triglyceride-driven remnant cholesterol burden.
- Best interpreted with blood pressure, diabetes status, coronary calcium score, and family history.
What are Atherosclerosis
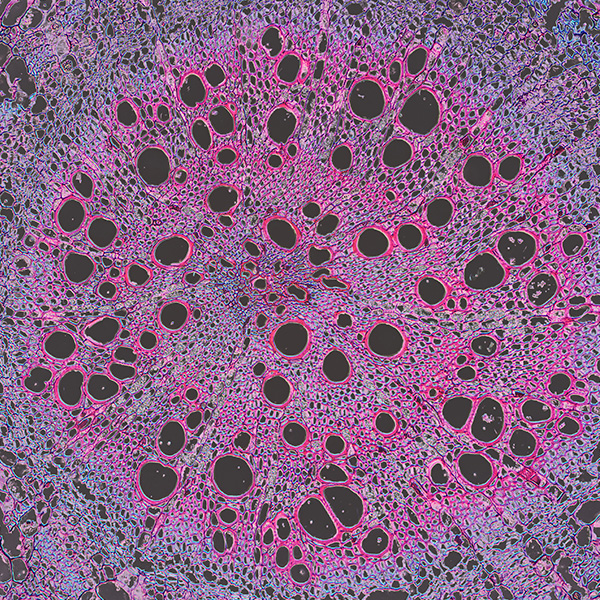
Atherosclerosis biomarkers are measurable signals in your blood that mirror what is happening inside artery walls as plaques form, grow, or become unstable. They capture the main forces that drive this disease: the burden of cholesterol-carrying particles (LDL cholesterol and apolipoprotein B; Lp(a)), smoldering vessel inflammation (high-sensitivity C-reactive protein; interleukins), oxidative injury (oxidized LDL), stress on the vessel lining (endothelial dysfunction markers), and the tendency to clot (fibrinogen; thrombin generation). Together, these markers reflect the balance between damage and repair in the arterial lining (endothelium and intima). Testing them helps surface risk before symptoms appear, estimate the likelihood of heart attack or stroke, and tailor prevention—what to focus on, how aggressively, and whether treatment is working. In short, atherosclerosis biomarker testing turns a silent, decades-long process into actionable information by translating biology into a risk signal you can track over time.
Why are Atherosclerosis biomarkers important?
Atherosclerosis biomarkers are the body’s traffic report for artery health: they track the number of cholesterol-carrying particles, inherited lipoprotein risks, and the level of vascular inflammation that drives plaque growth and instability. Because arteries feed every organ, these signals matter for the heart, brain, kidneys, and limbs.
Across common markers, “better” usually sits toward the low end of the reference range. LDL and ApoB reflect the count of atherogenic particles; lower values signal fewer particles entering the artery wall. Lp(a) is an inherited particle that accelerates plaque and thrombosis risk; lower is safer. hs-CRP gauges arterial inflammation; lower suggests calmer vessel walls. AIP (the balance of triglycerides to HDL) and AC (non-HDL relative to HDL) integrate lipid quality; lower values indicate a less atherogenic milieu. High values across these markers often remain silent for years, yet they track with plaque growth, angina, claudication, and stroke risk.
When these biomarkers are low, they reflect fewer particles, better reverse cholesterol transport, and quieter immune signaling—conditions that slow plaque formation and promote stability. Symptoms are usually absent. Very low LDL/ApoB can accompany hyperthyroidism, malabsorption, advanced liver disease, or rare genetic states; any symptoms stem from those conditions. Children and premenopausal women tend to have lower LDL/ApoB; hs-CRP runs slightly higher in women. Pregnancy physiologically raises lipids, so unusually low values are uncommon then.
Big picture, these markers link lipid transport, inflammation, and metabolism. Read together with blood pressure, glucose, kidney function, and family history, they forecast long-term risks for heart attack, stroke, and peripheral artery disease and illuminate how the whole system is handling vascular stress.
What Insights Will I Get?
Atherosclerosis biomarker testing reveals how lipoproteins and inflammation shape plaque formation, stability, and blood vessel health. This matters for energy delivery, heart and brain perfusion, kidney function, and immune tone. At Superpower, we test LDL, ApoB, Lp(a), hs-CRP, AIP, and AC.
LDL is the cholesterol carried within low-density lipoproteins; excess LDL fuels plaque growth. ApoB counts the number of atherogenic particles (LDL, VLDL, remnants) that can enter and be retained in the arterial wall. Lp(a) is an LDL-like particle with apolipoprotein(a); it is strongly pro-atherogenic and pro-thrombotic. hs-CRP is a high-sensitivity measure of systemic and vascular inflammation that accelerates plaque progression. AIP (log of triglycerides to HDL-C) reflects the burden of triglyceride-rich remnants and small, dense LDL. AC ((total cholesterol − HDL-C) divided by HDL-C) expresses the balance between atherogenic and protective lipoproteins.
For stability and healthy function, lower LDL and ApoB indicate fewer particles available to infiltrate arteries, supporting endothelial integrity and calmer plaque biology. Lower Lp(a) suggests less inherited, residual risk of plaque growth and thrombosis. Lower hs-CRP points to a quieter inflammatory milieu, associated with thicker fibrous caps and reduced plaque vulnerability. Lower AIP and AC imply larger, less penetrant LDL particles and stronger reverse cholesterol transport, favoring vessel resilience and nitric oxide–mediated vascular function.
Notes: Lipids rise in pregnancy and with aging; menopause shifts patterns. Acute infection, injury, and chronic inflammatory disease elevate hs-CRP. Fasting status affects triglycerides and thus AIP. Medications and alcohol can alter all measures. Assays differ, especially for Lp(a) isoforms; hs-CRP requires high-sensitivity methods. Repeat measurements and clinical context improve interpretation.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


