Key Benefits
- Spot acute kidney injury early by checking filtration and waste buildup.
- Flag dehydration versus intrinsic kidney damage using the BUN/creatinine ratio.
- Explain fatigue, swelling, reduced urine, or confusion by confirming kidney stress.
- Guide urgent steps: fluids, imaging, or nephrology consult when numbers worsen.
- Protect kidneys by adjusting doses of antibiotics, diabetes drugs, and pain relievers.
- Protect fertility and pregnancy by optimizing kidney function and medication safety.
- Track recovery or relapse with repeat creatinine and BUN trends over days.
- Best interpreted with urine output, electrolytes, and your symptoms over time.
What are Acute Kidney Injury
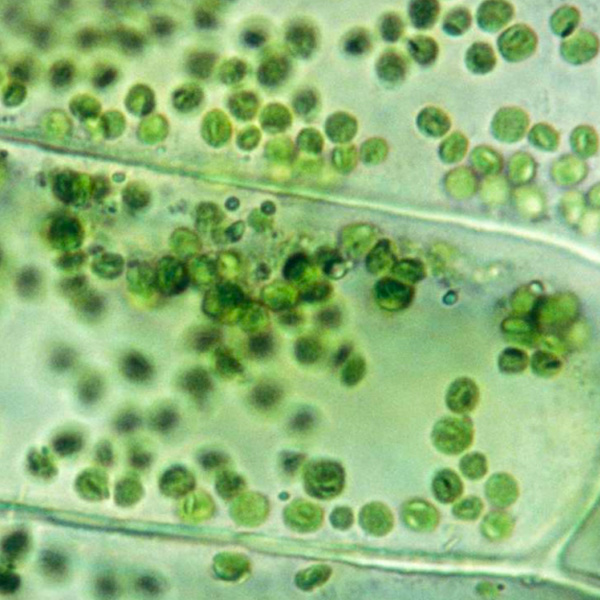
Acute kidney injury (AKI) biomarkers are signals in blood or urine that show how the kidneys are handling stress and damage in real time. Some reflect slowing of the kidney’s filter (glomerulus), such as creatinine and cystatin C. Others are released directly by stressed tubule cells, like the protein NGAL (neutrophil gelatinase–associated lipocalin), the injury receptor KIM‑1 (kidney injury molecule‑1), the stress markers TIMP‑2 and IGFBP7 (cell‑cycle arrest proteins), and the inflammatory signal IL‑18 (interleukin‑18). Together they reveal three states: early cellular stress before function drops, actual tubular injury, and loss of filtration. Because these molecules arise from kidney tissue or build up when filtering slows, they enable earlier detection of AKI, a clearer sense of severity, and insight into the dominant process (stress, injury, or impaired function). This matters because it turns hidden kidney distress into measurable signals, guiding timely decisions while the kidneys still have a chance to recover.
Why are Acute Kidney Injury biomarkers important?
Acute Kidney Injury biomarkers are the body’s early warning lights for filtration, fluid balance, electrolytes, and acid–base control. When kidneys falter, wastes and water accumulate, potassium and acids rise, blood pressure swings, and signals ripple to the heart, brain, lungs, and immune system. Tracking creatinine, estimated GFR, BUN, and the BUN/creatinine ratio shows how fast and how well the kidneys are clearing the bloodstream right now.
Creatinine typically sits around 0.6–1.3, with men a bit higher and women, children, and pregnancy lower due to muscle mass and physiologic hyperfiltration. eGFR is healthiest near the high end (about 90 or higher). BUN often falls near 7–20 and is most reassuring in the low–middle. The BUN/creatinine ratio clusters around 10–20, with “optimal” near the mid-teens.
When values run low, the meaning depends on the marker. A low eGFR signals reduced filtration and fits AKI: urine output may drop; swelling, shortness of breath, fatigue, nausea, and confusion can appear as fluid, acid, and potassium accumulate. In contrast, low creatinine usually reflects low muscle mass, dilution, or pregnancy/childhood physiology; it does not indicate AKI and can mask early injury because a small rise from a low baseline is still significant. Low BUN can accompany liver dysfunction, overhydration, or low protein intake and may blunt the BUN rise seen in dehydration. A low BUN/creatinine ratio can point toward intrinsic renal injury or low protein states.
Big picture: these biomarkers integrate kidney function with cardiovascular stability, toxin clearance, drug handling, red blood cell production, bone–mineral balance, and immune response. Persistent abnormalities predict complications, hospitalizations, and dialysis risk; timely interpretation helps prevent multi‑organ stress and safeguards long‑term health.
What Insights Will I Get?
Acute kidney injury (AKI) disrupts fluid balance, electrolyte control, acid-base regulation, toxin clearance, and blood pressure—systems that underpin energy, cognition, cardiovascular stability, and immune competence. At Superpower, we test Creatinine, eGFR, BUN, and the BUN/Creatinine Ratio to detect and characterize AKI.
Creatinine is a muscle-derived waste filtered by the kidneys; an acute rise signals reduced filtration. eGFR is a calculated estimate of filtration based on creatinine; lower values reflect reduced kidney function, though estimates are less reliable when function is rapidly changing. BUN (blood urea nitrogen) reflects protein metabolism and renal clearance; it increases with impaired filtration or increased nitrogen load. The BUN/Creatinine Ratio helps distinguish patterns of AKI related to hemodynamics (pre-renal) versus intrinsic renal injury.
For stability and healthy function, a stable creatinine with an expected eGFR indicates steady glomerular filtration. A rising creatinine with a falling eGFR indicates acute loss of filtration capacity; the pace of change reflects severity. Concurrent elevations of BUN and creatinine indicate retention of nitrogenous waste; a disproportionately high BUN with modest creatinine suggests reduced kidney blood flow or increased protein breakdown, whereas a lower ratio with high creatinine leans toward intrinsic tubular injury. Consistent, improving values suggest recovery; worsening trends suggest ongoing stress or injury.
Notes: Interpretation is influenced by age, pregnancy, muscle mass, acute illness, volume status, gastrointestinal bleeding, and catabolic states. Medications can affect creatinine secretion (e.g., trimethoprim, cimetidine) or renal hemodynamics (e.g., NSAIDs, ACE inhibitors, diuretics). eGFR equations and assays vary by lab and assume steady state.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


